Medically Reviewed by Katelyn Jetelina, PhD, MPH
Vaccines are vital public health tools that keep dangerous diseases in check. But how well they work depends on how many people receive them. In the U.S., socioeconomic and racial disparities, information gaps and lack of access to care have created an uneven landscape of vaccine uptake, which threatens public health.
Obstacles to vaccination
Despite their importance, vaccines aren't readily available for everyone and may be especially difficult to access for people of low socioeconomic status. Staying up to date on vaccines can be an expensive ordeal for those without health insurance. Some people decline vaccines due to financial reasons, and physicians may not recommend vaccines for certain patients due to their financial status and/or lack of insurance coverage.
Most private insurers must cover recommended vaccines with no copay, but if receiving the vaccine at a doctor's office (instead of a pharmacy), the visit may come with a copay.
Public insurance provides patchier coverage for vaccines. The states determine adult vaccine coverage for Medicaid enrollees, and only 22 states cover all recommended vaccines for adults. Medicare Part B covers certain vaccines at no cost, but costs for vaccines covered by Part D varies. Children can receive recommended vaccines at no cost through the federally funded Vaccines for Children program (VFC), but many remain unaware of this initiative.
Location can be another obstacle. For people who lack adequate transportation, getting a needed vaccine can turn into an hours-long affair and cause them to miss work. If a person moves frequently, it might be challenging to locate the family's vaccination history. These factors also make it harder for parents to take their children to regular well-child visits, where children can get needed vaccines.
These issues are complicated by booster shots, additional vaccine doses needed to boost immunity. Both the Pfizer-BioNTech and Moderna COVID-19 vaccines authorized by the U.S. Food and Drug Administration require a second dose a few weeks after the first. After the first dose, individuals are only partially protected from the disease. It's too early to say how delaying the second COVID-19 dose would affect immunity, but for some vaccines, missing the window for the next dose can mean starting that vaccination schedule all over again.
In recent years, lack of information or too much inaccurate information have emerged as important issues affecting vaccination rates. Both providers and patients need to understand the importance of vaccines to individual and public health, as well as how to access vaccines at little to no cost. This is particularly important in light of misinformation spread by the anti-vaccine movement, which has played a major role in the drop in childhood vaccine uptake.
Who gets vaccinated
Obstacles to vaccine uptake help perpetuate existing health disparities. A Centers for Disease Control and Prevention (CDC) report shows that in 2018, uninsured children aged 19 to 35 months had lower vaccine coverage than those on Medicaid or private insurance, and those on Medicaid had lower vaccine coverage than those on private/other insurance — despite the fact that free vaccines are available for children through VFC.
A 2018 CDC survey shows lower vaccine coverage among Black, Hispanic and Asian adults compared to white adults for certain vaccines. These disparities stemmed from a variety of factors, including access to care, insurance coverage, quality of care, attitudes toward vaccination and concerns about vaccine safety.
Where to find affordable vaccines
There are systems meant to ensure everyone can receive the vaccines they need, even without insurance. For example, the VFC program provides recommended vaccines to children under 19 who qualify for Medicaid, who can't afford the out-of-pocket costs of vaccines or who are members of Native American and Alaska Native communities.
Most public and private health insurance plans cover at least some recommended vaccines for adults at little or no cost. But vaccine coverage varies by state for Medicaid beneficiaries. Individuals should contact their state Medicaid agency to find out what's covered. When insurance coverage falls short, people can turn to other resources. Some pharmacies might offer discounts, and local health departments may offer free or low-cost vaccines. Federally funded health centers might also offer vaccines on a sliding pay scale.
The COVID-19 vaccine initiative ensures that Americans will not have to pay for the vaccine itself. Providers may charge administrative fees, but public and private insurers can reimburse vaccination providers for those administrative costs. The Health Resources and Services Administration's Provider Relief Fund can also reimburse providers for uninsured patients.
However people receive and pay for their vaccines, the federal, state and county programs providing free and low-cost vaccines need to run smoothly to show the public that these systems work and offer vaccine access for all.
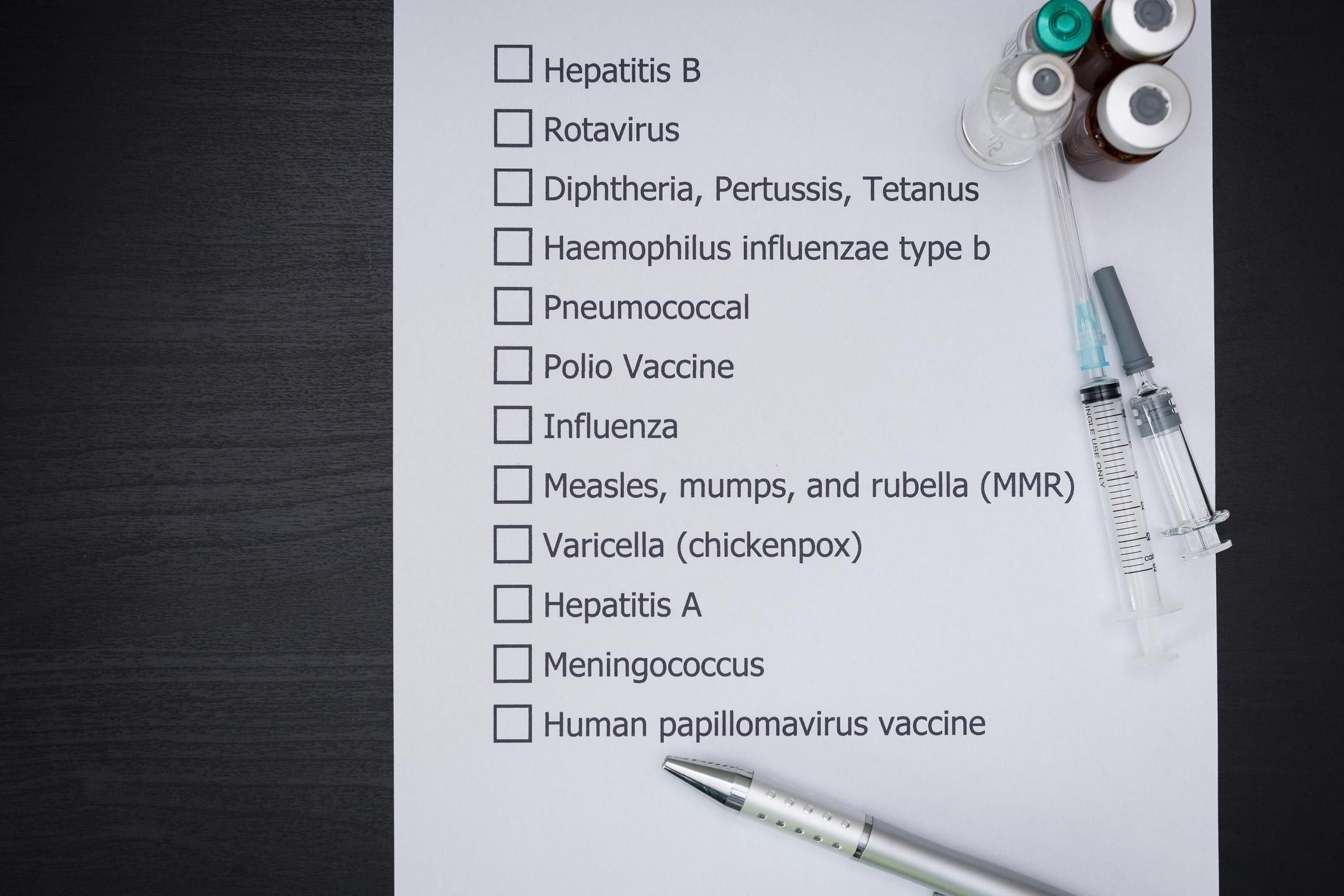
How to prioritize your vaccines
If, despite these resources, under- and uninsured women struggle to find free or low-cost vaccinations for themselves, there are vaccines that take priority depending on your age and health status. The CDC states that all adults need annual flu vaccines and should get the Tdap (tetanus, diphtheria and acellular pertussis) vaccine if they did not receive it earlier. Adults also require a booster shot for tetanus and diphtheria every 10 years.
While recommended vaccines can vary by an individual adult's health status and work or school requirements, the CDC recommends prioritizing certain vaccines for younger and older adults.
Adults 19 to 26 years old should receive the human papillomavirus (HPV) vaccine if they did not receive the vaccine as an adolescent. This vaccine helps protect women from viral strains that can cause cervical cancer, vaginal cancer and vulvar cancer. Depending on a patient's risk for HPV infections, the vaccine can be given in older adults up to age 45.
Adults over 50 should receive the shingles vaccine and adults over 65 should receive the pneumococcal vaccines PPSV23 and PCV13. The pneumococcal vaccines protect against meningitis and bloodstream infections, pneumonia and other infections caused by pneumococcal bacteria.
The CDC also recommends that those who are pregnant receive the Tdap vaccine during each pregnancy. The complete adult immunization schedule and child immunization schedule can be found on the CDC site. The CDC's Adult Vaccine Assessment Tool also can show you what vaccines you might need.
Vaccines are incredibly important to individual health and to public health. It is important to ask about vaccines you and your family members might need and, if cost is a problem, to ask how they can be covered. Systems have been put in place to ensure vaccines are available to all who need them at no cost. No one should have to decide which lifesaving vaccines take priority.
This resource was created with support from Merck.