Just because something is well known, doesn't mean it's well understood. This is the case with endometriosis. The disease is one of the most common gynecologic disorders in America, affecting an estimated one in 10 women, yet there is a lack of awareness and prioritization of endometriosis as an important women's health issue.
Endometriosis Misunderstood
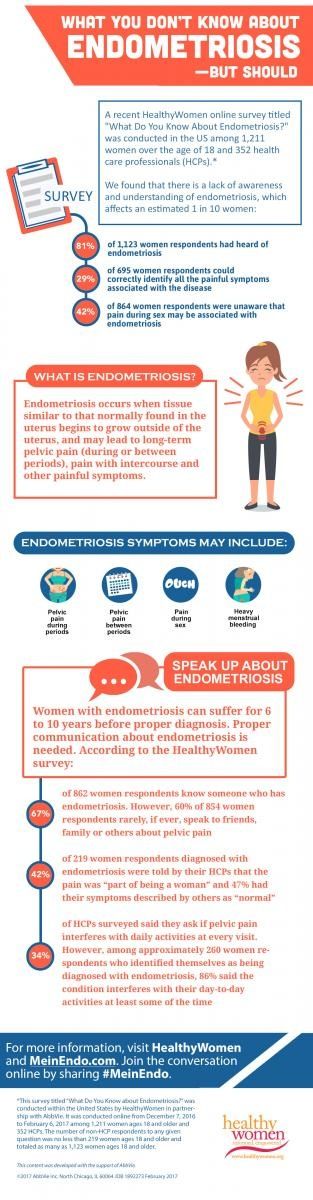
However, among almost 700 respondents, only 29% were able to correctly identify all the painful symptoms associated with the disease, including painful urination or painful bowel movements. In addition, 42% of more than 850 women respondents were unaware that pain during sex may be associated with endometriosis, and 20% of HCPs surveyed rarely or never ask female patients if they have pain during sex, even though it is a common symptom of endometriosis.
Nearly half (45%) of about 850 women respondents didn't know if there was a cure for endometriosis (answer: there isn't). Among approximately 800 respondents, only 36% identified laparoscopic surgery as a way to diagnose endometriosis, even though a laparoscopy to remove a small sample of tissue for testing, known as biopsy, can confirm an endometriosis diagnosis.
Communication Breakdown
A lack of understanding of how to identify symptoms of endometriosis and how to address them can lead to miscommunication when speaking about symptoms with an HCP.
Among 850 women respondents, approximately 37% identified themselves as diagnosed with endometriosis. Of those, 219 women responded to additional questions about their symptoms, and 42% were told by their HCPs that their pain was simply "part of being a woman," while 47% had their symptoms described by HCPs as "normal."
The communication issues are not, however, all one-sided. Only 43% of HCPs surveyed said they are very comfortable when it comes to managing female patients with chronic pelvic pain. HCPs reported they are more likely to consider endometriosis as a possible cause of chronic pelvic pain than as a possible cause of first-time acute pelvic pain.
Only 34% of HCPs surveyed said they ask if pelvic pain interferes with daily activities at every visit. However, among approximately 260 women respondents who identified themselves as being diagnosed with endometriosis, 86% said the condition interferes with their day-to-day activities at least some of the time.
When asked to identify with some common challenges associated with endometriosis, women respondents cited heavy menstrual bleeding as the most challenging problem created by endometriosis. Other challenges included not being able to participate in routine activities due to pain, missing work, painful sex and feeling alone after the diagnosis.
This communication breakdown speaks to the need for providers to be more aware of evaluating and treating symptoms. Women should also feel empowered to share their symptoms to help ensure key information about endometriosis indicators is not left out during appointments with HCPs. Among 862 women respondents, two-thirds (67%) know someone who has endometriosis, but the majority (60%) said they rarely, if ever, speak to friends, family or those closest to them about pelvic pain.
Diagnosis Delay
Among approximately 260 women respondents who identified themselves as diagnosed with endometriosis, pain during or before periods was the most common symptom to lead them to see their HCP. Nearly half (45%) of those respondents with endometriosis took four or more years to see an HCP about their symptoms and 28% took seven years or more.
Without proper communication about endometriosis, it may take longer for women to receive a proper diagnosis. Women with endometriosis can suffer for 6 to 10 years before diagnosis. In fact, among approximately 260 women respondents who identified themselves as diagnosed with endometriosis, 72% had to see two or more HCPs, and 24% saw four or more before receiving a diagnosis. Nearly a quarter (23%) of respondents with endometriosis waited four or more years to receive a diagnosis.
Once diagnosed, there is no one-size-fits-all approach to treatment for this disorder. In fact, women respondents with endometriosis reported using a variety of treatments—medical, surgical and other—to manage their endometriosis symptoms. Among 258 women respondents with endometriosis, approximately 39% have used some form of medical treatment, including oral contraceptives, anti-inflammatory drugs and gonadotropin-releasing hormone agonists.
Speak Up
If you have pelvic pain or other symptoms of endometriosis, the first step is to talk to your HCP.
Before your appointment, arm yourself with knowledge. Gather your medical records and write down your symptoms. Websites such as MeinEndo.com offer helpful tools including an endometriosis checklist and symptom tracker, which can help you log how much pain you experience on an average day and how often; if there's a time of day when symptoms are worse or better; if specific activities worsen or relieve the pain; or if the pain comes and goes.
Don't downplay your symptoms or be afraid to ask questions. It's also important to find an HCP who has experience treating endometriosis.
Among 766 women respondents—diagnosed or not with endometriosis—nearly three-fourths (73%) said they wanted more information on this disease. Educational resources like HealthyWomen and MeinEndo.com can provide women with reliable information to learn about and better understand endometriosis.
*This survey titled "What Do You Know about Endometriosis?" was conducted within the United States by HealthyWomen in partnership with AbbVie. It was conducted online from December 7, 2016, to February 6, 2017, among 1,211 women ages 18 and older and 352 HCPs. The number of non-HCP respondents to any given question was no less than 219 women ages 18 and older and totaled as many as 1,123 women ages 18 and older.
- FAQs: What You Need to Know About Endometriosis ›
- True or False: Endometriosis ›
- It Took 3 Decades for Me to Receive an Endometriosis Diagnosis - HealthyWomen ›
- Why Getting an Endometriosis Diagnosis Is Painfully Slow - HealthyWomen ›
- My Hysterectomy to Cure Endometriosis Wasn't the Right Decision - HealthyWomen ›
- My Treatment Options for Endometriosis Were Unacceptable - HealthyWomen ›