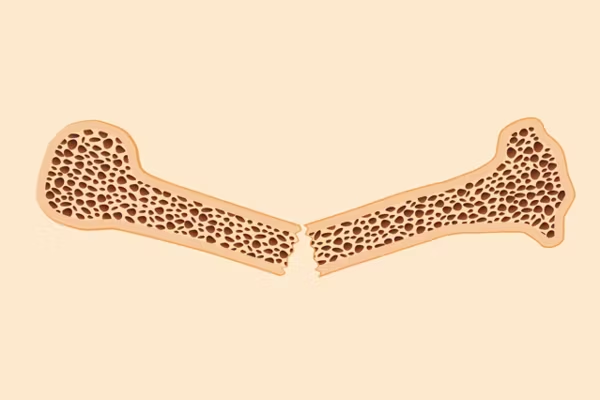
A woman’s risk of fracturing her hip from osteoporosis is equal to her risk of breast, uterine and ovarian cancer — combined. And half of all women in the United States who are over age 50 will break a bone as a result of osteoporosis, a condition that occurs when your bone quality declines and bone weakens.
Osteoporosis can make it so easy for your bones to break that even everyday movements such as stretching, twisting, bending too far backward or forward, coughing, or bumping into something can be a danger. This can be serious because broken hips can lead to a shorter lifespan, and broken spines can cause an inability to stand up straight, paralysis or, sometimes even death.
One in five women over age 50 will develop the bone condition in their lifetime, so HealthyWomen recently conducted a survey of 1,072 women between the ages of 35 and 64 to assess awareness of the disease as well as knowledge of screening for and prevention of this common condition.
As with so many diseases, awareness and prevention are key to better outcomes when it comes to osteoporosis, yet our survey revealed that only one in four of our respondents were concerned about their bone health.
DEXA scan — a measure of bone health
Dual energy X-ray absorptiometry, called a DEXA or DXA scan, measures bone mineral density (BMD) and is recommended for everyone above age 65. However, healthcare providers (HCPs) may recommend a DEXA scan earlier if they have a reason to suspect or want to rule out osteoporosis or osteopenia, which is when a person has decreased BMD but it’s not low enough to be osteoporosis. Common situations where an HCP might order a scan at any age include:
- A family member with bone health issues
- A recent bone break
- Use of medicines linked to bone health issues
- Another diagnosis, such as cancer, that could compromise bone health
Since our respondents were under the age of 65, it’s not surprising that 81% of them didn’t know their bone density score. Of those who did know, the majority were respondents who are concerned about osteoporosis or osteopenia, including women who are taking medication for either condition.
Of our respondents who were diagnosed with breast cancer and advised that they were at risk for osteopenia or osteoporosis, 65% hadn’t had a DEXA scan in the past two years despite their increased risk.
Eshani Agrawal, 28, is an example of someone who has had a DEXA scan at a young age as a result of being in a high-risk category. She has ulcerative colitis, a disease of the colon, and has taken medicines to combat flare-ups that sometimes affect bone health. “Since I was at a relatively high dose, the doctor asked me to get a DEXA scan,” she said. “It appears that there may have been some damage done.” She explained that she’s frustrated that her bone health could be affected by medication and wonders if some tooth sensitivity might also be connected.
Donna Leslie, 65, has been on the lookout for bone health issues since she was 50 because her older sister and mother both have osteoporosis. When Leslie’s mother was in her 50s, she rolled her ankle and broke it. Aware of her mother’s history, Leslie got a DEXA scan at 53 to provide her medical team a baseline number so they could monitor her BMD through the years. The scan showed she already had osteopenia. Her HCP told her to get more calcium in her diet but didn’t take any other action. At 62, she had another scan and learned her score had dropped to -2.5, a score that indicates osteoporosis. Her HCPs then began aggressively treating her condition, prescribing annual infusions which, a few years later, have led to an increase in bone mass.
Only one in four women had been warned of possible bone loss
Just as Agrawal experienced bone health issues as a side effect from medication for other conditions, Anna*, 69, was diagnosed with osteopenia after a DEXA scan revealed low BMD scores in both hips. She had been taking a hair-loss medication that she hadn’t been told could affect bone health. Anna’s not alone in her surprise — the HealthyWomen survey revealed one in four women who were diagnosed with breast cancer were not advised by their HCPs that some medications, such as certain cancer therapies, as well as cancer itself, may put their bone health at risk.
Anna was also surprised by her low BMD because she was overweight, and she’d always thought osteopenia and osteoporosis are conditions that underweight or normal weight women develop, which isn’t necessarily true. Both she and Leslie have since learned that exercise can slow the progress of the disease and now walk regularly, among other measures such as eating calcium-rich foods and keeping up with HCP follow-up visits.
Unfortunately, our survey taught us that, despite osteoporosis being a common condition among women, many aren’t aware of the prevention and treatment strategies they can take to ward off the disease. It’s important for every woman to understand how they can keep their bones healthy and to learn more about bone health. Be sure to talk to your HCP about your particular risk.
*Anna is not her real name.
This resource was created with support from Amgen.
- How Women of All Ages Can Prevent Osteoporosis - HealthyWomen ›
- Osteoporosis and Fractures: What You Should Know - HealthyWomen ›
- Clinically Speaking: Questions to Ask Your Healthcare Provider ... ›
- Fast Facts: 10 Facts About Osteoporosis in Women - HealthyWomen ›
- Osteoporosis - HealthyWomen ›
- What You Need to Know About Osteoporosis - HealthyWomen ›
- Osteopenia Diagnosis - HealthyWomen ›
- Concerns About Osteoporosis Medication - HealthyWomen ›
- Questions to Ask Your Doctor About Bone Health - HealthyWomen ›
- Preguntas que debes hacer a tu doctor acerca de la salud ósea - HealthyWomen ›
- Facts About Women’s Bone Health - HealthyWomen ›