Emily Jamea, Ph.D., is a sex therapist, USA Today Best-Selling author and podcast host. You can find her here each month to share her latest thoughts about sex.
"I've lost my libido."
"He's never in the mood."
"I feel constantly rejected."
"It wasn't always like this. We couldn't keep our hands off each other in the honeymoon phase."
"I'm in a sexless relationship."
"Please, help me increase my desire!"
Desire is the most common, yet complex, issue that brings couples to sex therapy. I estimate that 90% of the phone calls I receive are from couples struggling with a difference in sexual desire. This was the problem Jacqueline and Zuri were desperate to solve when they called my office.
“I don’t know how much longer I can go on like this,” Zuri said. They’d been together for 15 years and married for 10.
They told a story I’d heard many times before. Things had been great in the beginning. They experienced a whirlwind romance after meeting at a cocktail party in London, where they were both attending a conference. They dated long-distance for the first year, and, like most couples who date long-distance, indulged in long weekends full of passionate sex whenever they got the chance. When it became clear they were falling in love, Jacqueline put in a request at her global company to relocate. She packed her bags and moved into Zuri’s tiny apartment in lower Manhattan.
“What were things like in those early years?” I asked.
“Naturally, things slowed down a little bit once we moved in together. I don’t think either of us expected to carry on the way we had the year prior.”
They looked at each other and laughed.
“I’d say we felt happy with our sex life for the first few years,” Jacqueline said. “It was always passionate and loving. It felt mutual. Zuri probably initiated more than me, but I don’t think either of us were concerned about that. It worked.”
She went on. “I don’t know what shifted. It used to feel so automatic, but that’s not the case anymore. I’m never ‘in the mood’ the way Zuri is. I can’t pinpoint anything that made me shut down. It seems like it just sort of happened gradually.”

“What has that been like for you?” I asked Zuri.
“It’s been incredibly painful. I feel rejected, alone and unloved. Sex is important to me. When weeks go by without sex, I can’t help but get prickly, which I know doesn’t help things,” Zuri said.
“That’s for damn sure,” said Jacqueline. “She starts pouting, which is a huge turnoff. Sometimes I give in just so she’ll be happy again, but I don’t think either of us feels good about that. It’s really deteriorated our relationship. I think we both feel like we’re walking on eggshells around each other. That alone kills my interest.”
“Tell me a more about what sex is like when you’re feeling closer in your relationship, assuming there are still some windows of connection.”
“It usually happens after spending a relaxing weekend together. Jaq’s job stresses her out, and I know she needs time to decompress. So we’ll take it easy, and usually I just ask her. I’ll say, Hey, what do you think about having sex today? And if she says yes, we do it.”
“And how is it when you do make love?” I ask.
“It’s still really good,” says Jacqueline. "It’s not like I don’t enjoy sex. I’m just never in the mood. It’s not as wild as before, but we both experience pleasure and satisfaction. And the best part is, the relationship is great the following week! Zuri is happy. We get along. But then time goes by.”
“Okay. I think I’ve got it. I believe you’re experiencing one of the most classic paradoxes of sexual desire. It sounds like Zuri is in the mood a lot and usually open to have sex, but you’re only in the mood when you feel relaxed and close to her, and even then, you don’t really get in the mood until you actually start having sex.”
“I never thought about it like that, but you’re right. Once we get going, I’m good. It’s just hard to get going,” Jacqueline said.
Jacqueline and Zuri were experiencing the fallout of not understanding the difference between spontaneous and responsive sexual desire. We are force-fed the idea that sexual desire should always be spontaneous, and that sex is only good if it’s unplanned. Most people subscribe to the idea that desire comes first, then arousal, then an orgasm, and then the whole process starts over again. That’s the “spontaneous model,” but that’s not the way it works for most people.
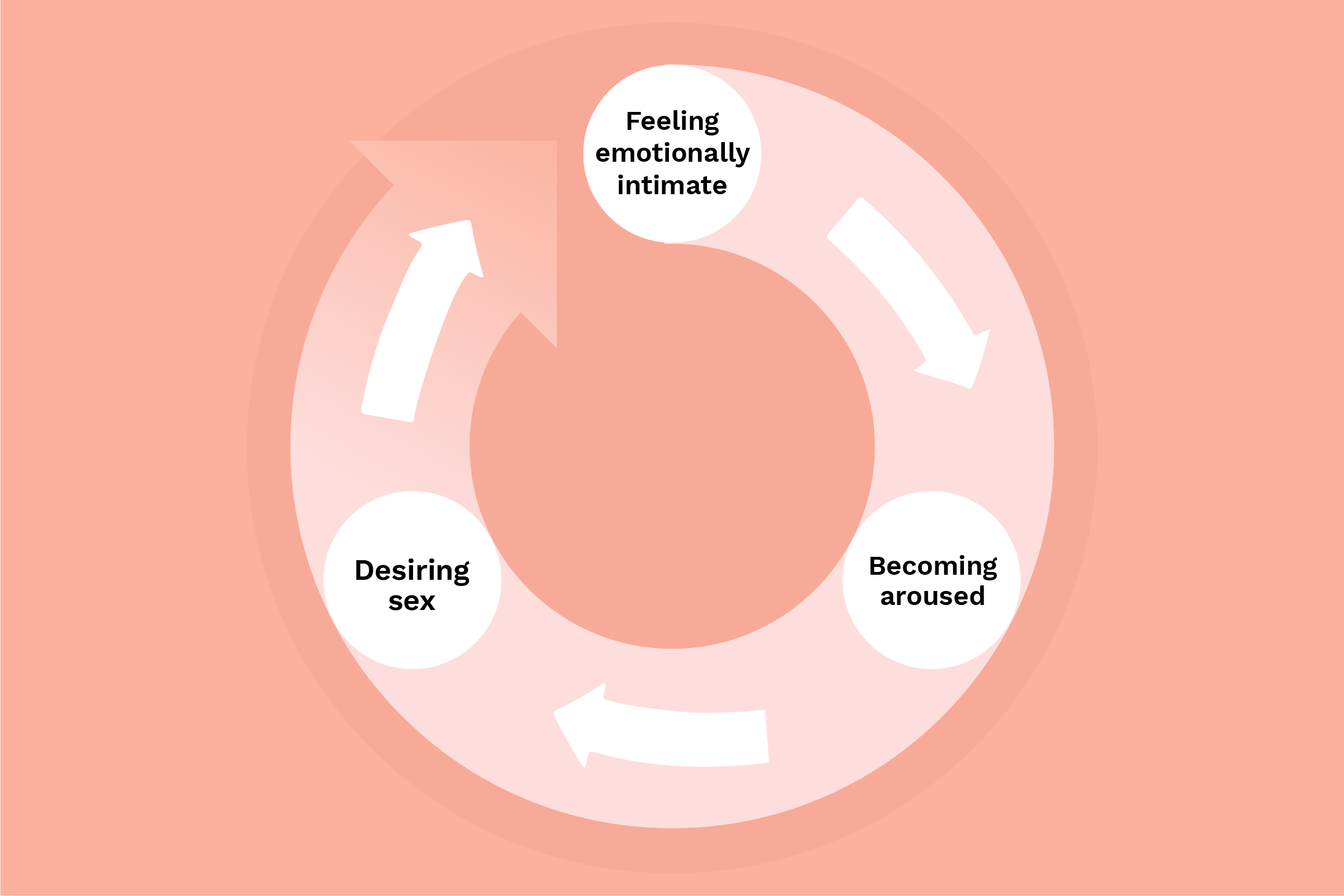
Rosemary Basson created what we now refer to as the “responsive model” for sexual desire. In this model, desire comes after feeling emotionally close to your partner and experiencing a little bit of sexual arousal. It’s not until the presence of those two things — emotional connection and arousal — that the desire for sex comes. The spontaneous model is linear. The responsive model is circular.
Zuri knows that Jacqueline is stressed out by her job. She takes extra care on the weekends to help Jacqueline relax, which makes Jacqueline feel loved and cared for. Seeing a window of opportunity, Zuri gently asks Jacqueline if she might be in the mood. Despite not being in the mood at that moment, Jacqueline notices that she at least feels open to the idea, so she agrees. Once they get going and she becomes aroused, she gets into it and then experiences desire.
I could see the pieces of the puzzle coming together for them.
“There’s nothing wrong with experiencing desire in different ways. They key is that you understand and respect each other’s differences and use your knowledge to work together in a way that feels mutually satisfying to you,” I told them.
They returned for a second visit a few weeks later.
“So how are things going?” I asked.
“Things have been so much better!” Zuri said. “I’m not going to lie, I still miss the days when Jacqueline initiated sex, but I feel like tension we were experiencing on a weekly basis has totally evaporated. I think there will always be a little bit of a difference in our libidos, but it feels manageable now.”
“How are things for you, Jacqueline?”
“I don’t feel broken anymore. I thought something was wrong with me. Just knowing I’m completely normal has given me such relief. Now I’m always assessing whether I’m at least open to the idea of sex, and with that new tool, I find that I’m open to the idea more than I initially realized. So I agree with Zuri, everything feels more manageable. And the relief I’m experiencing actually has led to a couple spontaneous moments. Remember last Thursday night, Z?”
Zuri’s smile said it all.
Names have been changed to protect privacy.







