By Brian Peppers, West Virginia University
Human beings are born pretty helpless, with a lot of developing to do. And just as you must learn such skills as how to walk, so must your immune system learn to defend against infections. As time passes, your immune system matures through different stages, much the way you advanced from crawling to standing, walking and running.
This process is one of the reasons scientists study the immune response to a vaccine in different age groups, and why, for example, the COVID-19 vaccines need to be tested separately in children ages 5-11 and those 12-16. Doctors want to use the vaccine dose that provides the best protection with the fewest side effects. And that's going to depend on how the immune system is working based on how developed it is – something you can't really tell from the outside.
I'm an immunologist, and here's the way I explain to my pediatric and adult patients how vaccines work in people of all different ages.
Two halves of the immune system
The immune maturing process starts shortly after birth.
When you're born, your main immune protection comes via antibodies your mother shared through the placenta and breast milk. They provide what's called passive immunity. Newborns' adaptive immune system – the part of your immune system that will make your own antibodies – isn't really up and running yet. The process gets started right away, but it can take years for the adaptive immune system to reach full maturity.
Luckily you're also born with what's called the innate immune system – and it lasts throughout your life. It doesn't need to learn in order to fight off infections and promote health as the adaptive immune system does. Without the innate immune system people would get sick a lot faster and more often.
The innate immune system starts with your skin and mucous membranes. Should any germs get past those physical barriers, it has enzymes just waiting to break down foreign organisms. Beyond that there are specialized cells looking for anything that is not you in order to kill intruders, while other cells called phagocytes gobble up invaders.
So the innate immune system is your body's first responder. It buys you a bit of time. Then your adaptive immune system comes in and joins the fight.
When you become immunized via a vaccine or infection, your adaptive immune system starts actively making antibodies of your own. They're proteins that act like suction cups and stick to viruses or bacteria to help the body get rid of the germs faster and prevent the infection from spreading. Antibodies are specialized to recognize and take down a particular intruder.
The adaptive immune system can learn a new infection or recall one that it has not seen in a long time.
Vaccines account for immune development
In the same way an infant will learn to walk even if you don't secure the stairways and pool areas for them, your immune system can learn to squelch an invading virus without a vaccine – but the chance of injury is much greater.
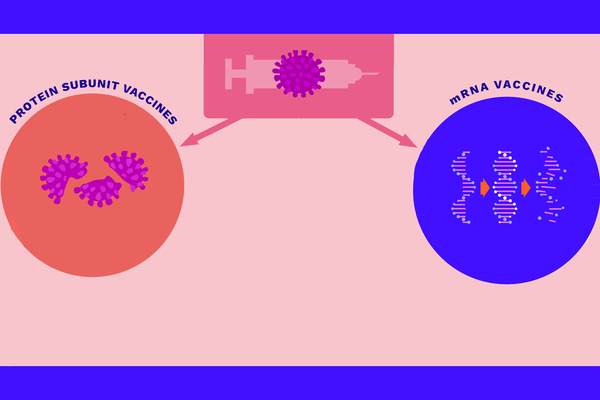
Vaccines work by triggering the creation of antibodies that will recognize a specific germ and work to fight it off in a safer manner than getting the infection for the first time without it. How well a vaccine works is a combination of how many antibodies you produce in response to it, how effective they are and the safety of the vaccine.
When researchers work to fine-tune the dosage of a vaccine for different age groups, they need to be aware of what parts of the immune system are online and what parts aren't fully active in people at each developmental stage. This is part of the reason some vaccines – such as for COVID-19 – get tested and approved on different schedules for adults, teens, kids and babies.
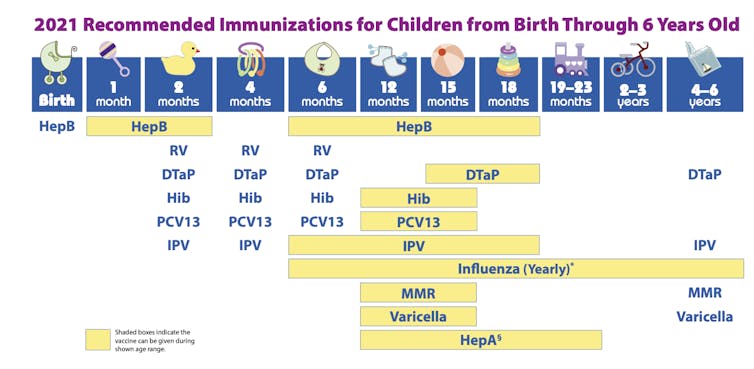
A number of vaccines for infants are given as a series – meaning they get the same kind of shot several times over the course of a few months. A baby's adaptive immune system is prone to being forgetful or not listening at this age – the same way a baby falters as it tries to stand and walk. With each exposure, every aspect of the immune system gets stronger and better at defending against the would-be infection.
Some vaccines need to be given multiple times.
CDC National Center for Immunization and Respiratory Diseases, CC BY
After 4 years of age and through younger adult life, your immune system tends to be more responsive and less prone to forgetting. It's not a coincidence that this is when people tend to gain most of their allergies. For the COVID-19 Pfizer vaccine, researchers found that kids ages 5 to 11 had a similar immune and safety response at one-third the dose used for those ages 12 and up.
Scientists tend to start with patients between ages 18 and 55 years old when studying vaccines. Their adult immune systems have matured and they can be counted on to reliably report any adverse reactions. Seeing what happens in the adult age group also helps physicians predict what might occur when a vaccine is administered to others and be on the lookout for these side effects in the younger age groups.
[Over 115,000 readers rely on The Conversation's newsletter to understand the world.Sign up today.]
Around age 55 or so, the adaptive immune system starts to become weaker again and forgetful, in some ways more like the infant's developing system. Luckily vaccine boosters can provide a quick refresher for these older patients – like helping protect them from accidental falls after a lifetime having mastered walking and running.
In the end, vaccines provide the safest environment for the immune system to learn, and tweaking the dosages for different age groups helps ensure that each patient gets just what's necessary to get the job done.![]()
Brian Peppers, Assistant Professor of Pediatric and Adult Allergy/Immunology, West Virginia University
This article is republished from The Conversation under a Creative Commons license. Read the original article.