By Claudia Finkelstein, Michigan State University
With the holidays approaching, many people are considering whether to visit relatives or friends in the coming weeks. At the same time, cases of COVID-19 are surging toward the highest levels since the beginning of the pandemic. As a physician, daughter of vulnerable seniors and mother of young adults, I have been thinking a lot about whether testing will help me decide if it's safe to see my family.
Testing may help you to make sure you and your loved ones stay healthy, but COVID-19 testing is not as simple as yes or no, infected or safe. There are many factors to keep in mind when using a coronavirus test to plan your holiday travels safely.
Some tests are better than others
Broadly speaking, there are two categories of tests.
Antibody tests – which look for evidence of previous infection – can't tell you whether you currently have COVID-19 and aren't useful for planning to visit family.
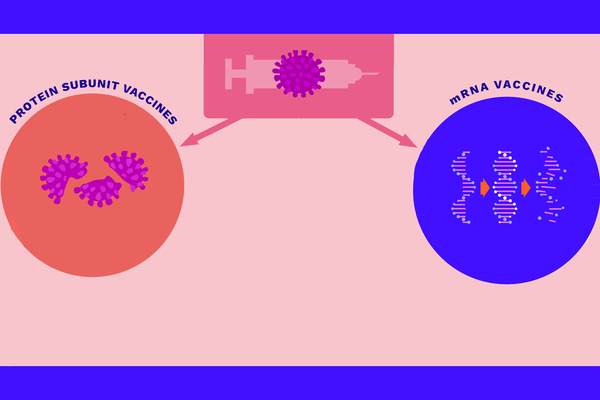
The other category of tests look for evidence of the virus in your body. There are two types of these viral tests available – RT–PCR tests and rapid antigen tests – and these are the ones to use when trying to prevent the spread of the coronavirus.
No lab test for COVID-19 is 100% accurate. Although false positives are certainly not a good thing, a false negative result – testing negative when you actually have the virus – is the bigger danger if you plan on seeing family. The false negative rates for RT-PCR tests range from 2%-29%. Much of that range is due to different manufacturers and user error. While fairly accurate, these tests often involve a visit to a health care provider and are somewhat expensive – around US$100, though costs vary widely by state – and it can take up to three days to get results. RT-PCR tests are the best tests available, but for some people, especially if you'll be seeing someone in a vulnerable age group, the high-end 29% false negative rate might leave more uncertainty than you are comfortable with.
Rapid antigen tests, in comparison, are faster and cheaper, but less accurate than RT–PCR tests. You can usually get results within a day of taking the test, but false negative rates can be as high as 50%. They are most likely to be accurate when they are given to people with symptoms within a week of symptom onset, but rapid tests are not meant to be diagnostic tests for an individual. They are much better at monitoring whole populations where people can be tested repeatedly, and quite frankly have little use as a one-time test.
With a rapid test you may get results instantaneously at a lower price, but they should not be the only thing to inform a travel decision. When the health of a family member is on the line, accuracy is your friend. RT–PCR tests are generally considered to be more accurate.
Timing matters
Regardless of which viral test you use, the results are accurate only for the moment when you were tested and reflect only the ability of the test to detect the virus. A negative result today of course doesn't prevent you from getting infected tomorrow.
But with the coronavirus, neither does a negative test mean you haven't been exposed to the virus. The time between coming in contact with the virus and beginning to shed infectious virus particles – the incubation period – varies anywhere between two and 14 days. For example, it's possible you could get exposed today, test negative tomorrow and then go on to be infectious a few days later.
Additionally, it is possible to spread the virus before you show symptoms – when you are presymptomatic – or even if you never develop any symptoms at all.
Minimize risk, accept uncertainty
First off, if you have any symptoms at all, stay home. If you do not have symptoms, then you can start to think about travel for the holidays.
Knowing that tests are imperfect, the safest thing you can do is to strictly self-quarantine for 14 days before your visit. Testing can offer a helpful data point, but a quarantine is the more foolproof option.
If you can't quarantine for a full 14 days, the next best thing is to limit potential exposure to the virus, isolate as much as possible as long as possible before you travel and get tested.
If you are worried about being an asymptomatic carrier and are unable to isolate, consider getting tested at least five days after your last possible exposure. This maximizes the chance of a test detecting the virus if you are infected.
Remember that traveling itself carries risk of exposure too. Driving with appropriate precautions – wear a mask, wash your hands and social distance – seems to be safer than flying.
The process of flying – the crowded airports, bus rides and close seating on the plane – is a serious exposure risk. Ideally, after flying you would self–isolate again at your destination for as long as possible and consider getting tested. That is a lot of time alone and waiting for test results, but I can think of no higher stakes than the safety of loved ones.
You’re not in it alone
Maintaining health is a group effort, and it takes only one infected person to cause an outbreak. Openly discuss the precautions that the people you are visiting are taking and the possibilities of social distancing during the visit.
[Get facts about coronavirus and the latest research.Sign up for The Conversation's newsletter.]
Remember that one negative test in a party of travelers is only that, one negative test. Just because you test negative doesn't mean you can assume that other people in your household are negative too. Everyone needs to get tested and follow the same isolation measures, as much of the spread occurring is happening at smaller private gatherings in close quarters.
Many people want to see our loved ones during the holidays. But there are enormous, life-and-death reasons to plan the visit carefully and to use information, isolation and testing wisely. You may decide that the risk is too high, and that is OK. But, if you decide to visit for the holidays, the safest option is a strict 14-day quarantine. Testing can help inform your decision, but is not the only thing that you should rely on.![]()
Claudia Finkelstein, Associate Professor of Family Medicine, Michigan State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.