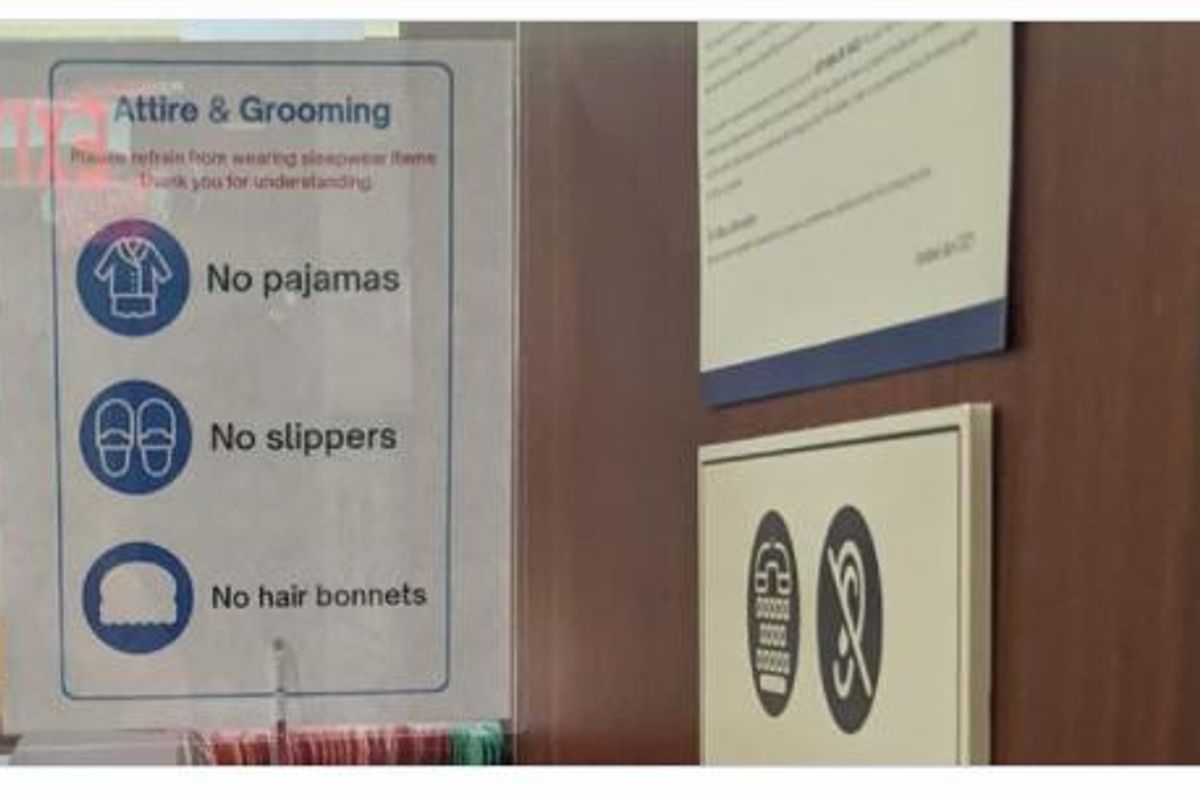
No pajamas. No slippers. No hair bonnets.
For some, the sign at a Columbus, Georgia, OB-GYN office could have been little more than a generic "no shirt, no shoes, no service" notice often spotted at public establishments. But Leslie Mac, a digital strategist, organizer and activist, saw something more insidious.

"This was a clear example of the types of unnecessary barriers to health care Black women have been noting for decades and that study after study have confirmed," Mac told HealthyWomen.org. "Black maternal health rates are abysmal in the United States and here we have a healthcare provider [HCP] putting stipulations on receiving care that are completely ridiculous."
Mac first saw the photo when it was shared in a private Facebook group, BonnetCon, designed to celebrate and uplift images of Black women. Outraged, Mac tweeted the photo, and it quickly went viral, with most responses echoing her sentiments. The majority of commenters raised points about the contradictory nature of an HCP posting a sign with language implying that certain groups of Black women could be denied care, all while Black women experience a maternal mortality rate 3.5 times higher than that of white women.

(Note: Mac incorrectly identified the location as being in Ohio but corrected it in later tweets.)
While the sign didn't specifically identify a particular racial or ethnic group, Mac said the language chosen was what is called coded language — when certain words are used to disguise explicit racism — and they sent a message to an intended audience.
"What is the difference between a bonnet and a headscarf?" Mac said. "A bonnet and a baseball cap? A bonnet and a turban? The difference is that primarily, it's only Black women who wear bonnets to protect our hair. Too often when Black women speak up about how we are treated, we are ignored — or worse gaslit — by being told we're making things up or making things sound worse than they are."
Deadly assumptions
Bruce McIntyre will always wonder if bias is the reason he lost his partner, Amber Isaac, when she gave birth a month early in April 2020. McIntyre said Isaac was well informed about the risks of pregnancy and the higher mortality rate for Black women, but she felt mistreated and annoyed by her HCPs at two facilities in the Bronx, which serve a largely Black and Latinx clientele.
Isaac went as far as documenting her feelings on social media, which McIntyre said came in response to not being seen by doctors in person for two months due to the COVID-19 pandemic

This was serious because Isaac had a low platelet count that needed to be monitored, McIntyre said, and her case required more than virtual prenatal appointments. He said her earlier blood tests had gone missing, and she was finally told to come in person to get bloodwork redone in mid-April. The next day, she was told to return immediately for treatment because her platelet count had dropped significantly.
McIntyre said Isaac was admitted April 20 for an induction and was diagnosed that day with a severe form of preeclampsia called HELLP syndrome, pushing doctors to order an emergency C-section. McIntyre was unable to be present in the operating room due to Covid-19 protocols.
He said he was told her low platelet count prevented her blood from clotting when the operation started, and that doctors tried to save her by massaging her heart, to no avail.
Today, McIntyre is an advocate for maternal health, creating the SaveARose Foundation in Isaac's memory. He's communicated with many families who've lost loved ones due to pregnancy or postpartum complications.
"The more I hear the stories, I start to see patterns of things going on within the medical system," he said. "It feels like they're not really giving women options. They're pushing a sense of urgency to confuse women, to make women feel like they have to consent or that they have to go with this or that procedure."
Identifying and addressing bias
With her experience working in healthcare settings around the country, Dr. Jessica Shepherd, an OB-GYN at Baylor University Medical Center in Dallas, is well aware of how patients can be treated differently due to provider bias. And bias isn't necessarily about race alone — the intersection of race and class and how both are perceived can contribute to health inequities.
"There are moments where we've seen a lack of understanding of differences in culture and we find ways to ostracize or isolate people from these cultures," she said. "By denying someone their right to receive healthcare based on their dress, it can be a bigger issue because of what we're seeing in maternal mortality with women from a specific group. This should be the real focus of how a policy like this can impact a group of people in healthcare."
That impact can also be seen through studies showing that healthcare providers falsely believe Black patients have higher pain thresholds or that way Black patients in pain are more likely to be depicted as potential addicts compared to white drug-seeking patients. For Black women in OB-GYN settings, delayed and denied treatment for reproductive issues and pregnancy-related care can be deadly, as illustrated by Isaac's heartbreaking death.
Mac's tweet attracted the attention of Georgia state representative Renitta Shannon, who called the hospital group that runs the OB-GYN group with the "No hair bonnets" sign. Mac said Shannon told her the sign was put up "without their knowledge and immediately taken down," and Mac said she's continuing to work with Shannon to ensure it doesn't happen again.

McIntyre's work also continues.
"Nobody should have to feel what I'm feeling," he said. "Nobody should have to go through what I'm going through. And I'm just thinking about my son Elias and how this is going to play out for his future without having his mother. I know I can't let this happen to anyone else. I can't let this happen to other families."
- Declaring racism a public health crisis brings more attention to ... ›
- Bias, Chronic Pain and Access to Care - HealthyWomen ›
- Trying to Avoid Racist Health Care, Black Women Seek out Black ... ›
- What Is Race-Based Medicine? - HealthyWomen ›
- Suffering From Chronic Pain as a Black Woman ›