As told to Nicole Audrey Spector
When I was a baby, I was diagnosed with beta thalassemia, a rare blood disorder that makes you unable to produce enough healthy red blood cells.
Back then, the only way for me to survive was to receive regular blood transfusions. I had my first one at just 8 months old, and had them every three to four weeks for many years to follow.
A side effect of being transfused so often is iron overload, which can lead to a number of health problems, including kidney and liver issues. By the time I was 5, I had to be on medication to lower the excess iron. At the time, this medication could only be given through injections. I started with a port and eventually got an IV pump, and my parents would put a needle in my stomach five to six nights a week.
I had to sleep with the medicine pumping through me, which meant not being able to sleep over at friends’ houses. It was a lot of responsibility for a little kid.
Fortunately, by the time I graduated high school, I was able to get an oral version of the medication. I went off to college three hours away from home. I chose a university that was near a hospital, so I could continue to get my monthly blood transfusions. Requiring transfusions so often in college was tough. I had to work my class schedule around them and always remember that for an entire day every month, I’d be getting transfused and have no room to do anything else that day.
I would get so tired leading up to the transfusions. Then I’d feel like a brand new person right after them.
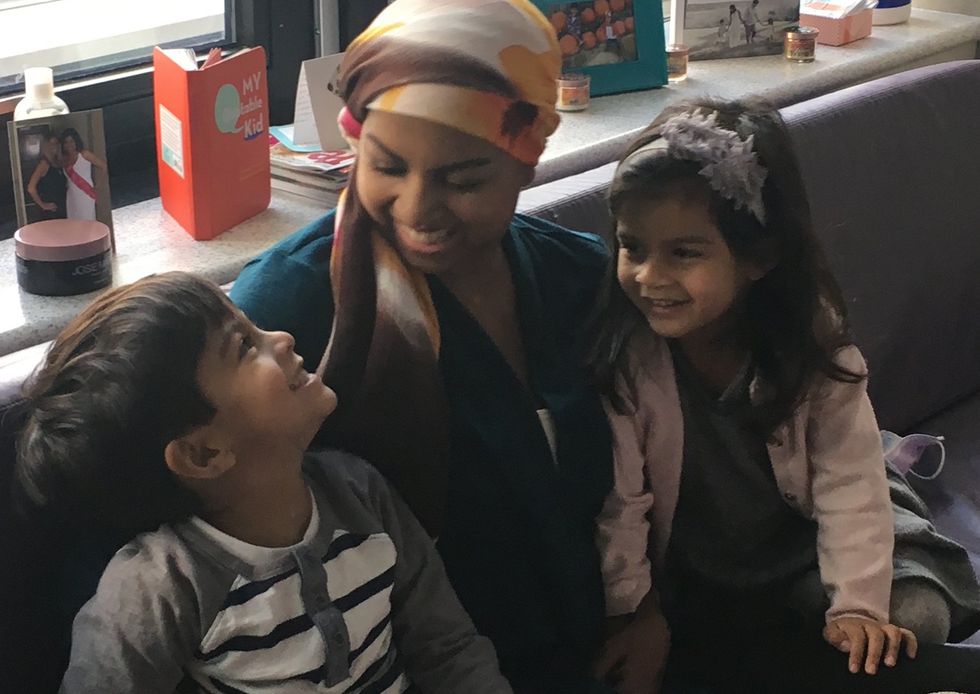
My life with regular blood transfusions continued — all through getting married and even throughout my two pregnancies. I nursed my babies while getting transfusions.
Living with beta thalassemia was doable, but so hard. Every time I blew out a birthday candle or tossed a penny in a fountain, I wished for the disease to be gone.
When I was 30, my beloved hematologist moved away and I got stuck with a new one who I really didn’t like. He wasn’t collaborative and didn’t respect that I knew my own body well enough to know when I needed a transfusion. He made me come in all the time so he could approve my blood transfusions, unlike my previous hematologist who trusted me to know my symptoms.
One day I posted in a Facebook support group for people living with beta thalassemia about how annoyed I was by my hematologist. Right beneath my post, I saw another one shared by someone about a clinical trial that used gene replacement therapy to treat people with my condition. The person was no longer transfusion-dependent because of the trial.
I clicked on the link to the trial, figuring, “Why not?” and filled out a form saying I was interested in learning more, not really thinking much of it.
A couple of days later, I got a call from the research coordinator at a hospital in Philadelphia. He asked if I'd like to learn more. I said I did.
Things moved fast from there. But throughout the journey, my family and I took each step one at a time.
I traveled to Philadelphia from Northern Virginia to have a number of tests so a team of doctors could determine whether I was eligible for the clinical trial. It turned out that I was. That meant I would undergo gene replacement therapy. And if the treatment was successful, I would no longer need blood transfusions.
Participating in the clinical trial would bring significant challenges. It meant staying in Philadelphia for up to a couple of months, three hours away from my family. It meant going through chemotherapy to kill all the cells in my bone marrow so that new cells would have room to grow and reproduce. It meant having a stem cell transplant, an invasive and intense procedure.
After talking it over with my family, we agreed that the clinical trial was worth exploring further. But even once I was in Philadelphia to begin the first steps of the process, I was torn. What if I didn’t get better after the trial? After all, not every eligible patient is guaranteed success. Far from it.
Randomly, I emptied my purse on my bed and discovered an old fortune cookie. As I held it, I desperately hoped that its message would give me direction. I opened it.
“Your dearest wish will come true,” it read.
I was disappointed. The fortune struck me as totally unhelpful. But later that night, it dawned on me. I remembered all those birthday candles I’d blown out and all those coins I’d tossed into fountains. The same wish every time. The wish to get well.
I got chills and instantly felt confident that the clinical trial was the right choice for me. No longer did I focus on all the rough things I’d have to go through. Instead, I focused on what wonders could await me on the other side of it all.
A few months later, I was admitted to the hospital to begin the trial. Over the next six weeks, I had chemotherapy and the stem cell transplant. Afterward, I spent an additional six weeks in a hotel room by myself. Because my immune system had been basically wiped out by the chemo, it was important that I stay away from others. Even the slightest cold could really hurt my health.

When I finally got home, it became clear that the trial had been a success. My red blood cell count rose and, for the first time in my life, it didn’t come down.
Almost exactly a year after this whole process began, I had my last blood transfusion. After a couple years of healing, I no longer needed the medication to combat excess iron.

Nearly eight years later, I continue to live a healthy life without the need for blood transfusions or medication targeted at treating beta thalassemia. I have the clinical trial to thank for all this. It’s been a dream come true — one I never thought was possible.
Though it’s important to understand that not everyone who goes through a clinical trial will see positive results, I think it’s just as important to recognize that one can also transform your life for the better.
Since being in the trial, I’ve become a resource for others considering gene replacement therapy for themselves or their children living with beta thalassemia. I’m so honored to be able to lend insight and maybe, just maybe, be the fortune cookie others are looking for.
Resources
AstraZeneca COVID-19 Clinical Trial Materials for Immunocompromised People
Español
- ¿Es seguro participar en un ensayo clínico si eres inmunodeficiente?
- Soy inmunodeficiente y un ensayo clínico cambió mi vida
COVID-19 Clinical Trials
- A study for the protection of Covid-19 in people with impaired immune system (SUPERNOVA)
- A Nasal Treatment for Covid-19
- A study to Evaluate EDP-235 in Non-hospitalized Adults With COVID-19 (SPRINT)
Clinical Trials for Immunocompromised People
This resource was created with support from AstraZeneca.
Have a Real Women, Real Stories of your own you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
- Clinical Trials ›
- Why Diversity in Clinical Trials Is Important ›
- Why We Need More Black and Hispanic Women in Breast Cancer Clinical Trials ›
- What You Need to Know About Clinical Trials ›
- Immunocompromised People and Covid-19 Clinical Trials - HealthyWomen ›
- Personas inmunodeficientes y ensayos clínicos del covid-19 - HealthyWomen ›
- Congressional Briefing: Women in Clinical Trials - HealthyWomen ›