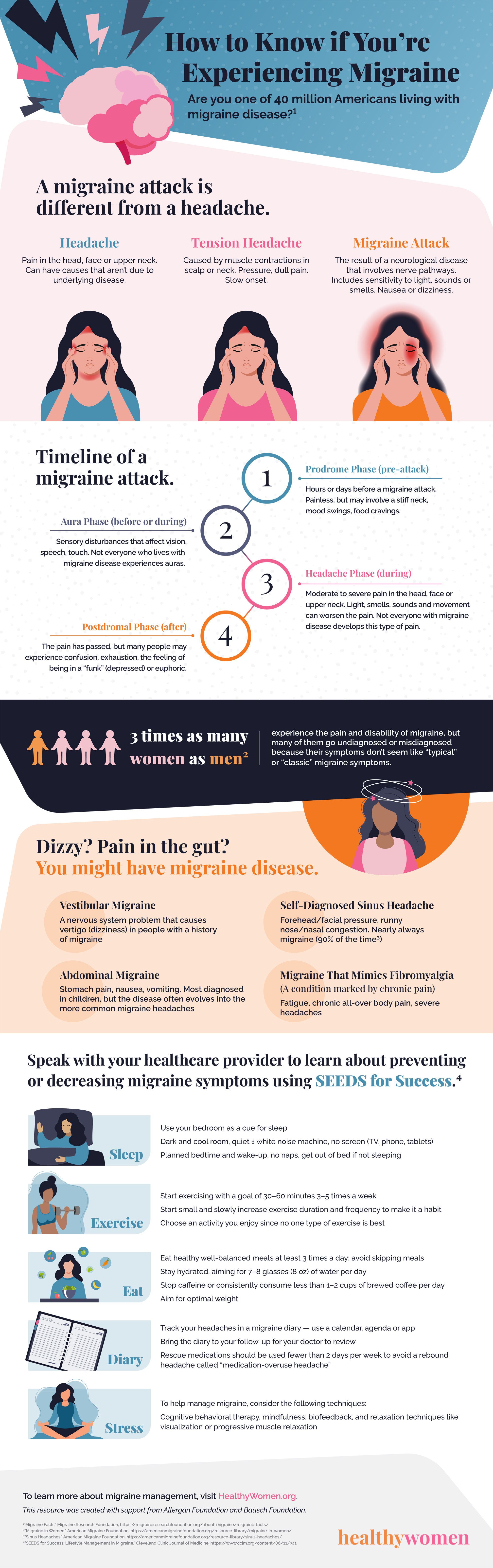
A migraine attack is
different from a headache.
Headache Tension Headache Migraine Attack
Pain in the head, face or upper neck. Can have causes that aren’t due to underlying disease.
Caused by muscle contractions in scalp or neck. Pressure, dull pain. Slow onset.
The result of a neurological disease that involves nerve pathways. Includes sensitivity to light, sounds or smells. Nausea or dizziness.
Timeline of a
migraine attack.
Aura Phase (before or during)
Sensory disturbances that affect vision,
speech, touch. Not everyone who lives with
migraine disease experiences auras.
Postdromal Phase (after)
The pain has passed, but many people may
experience confusion, exhaustion, the feeling of
being in a “funk” (depressed) or euphoric.
3 times as many
women as men2
Dizzy? Pain in the gut?
Prodrome Phase (pre-headache)
Hours or days before a migraine attack.
Painless, but may involve a stiff neck,
mood swings, food cravings.
Headache Phase (during)
Moderate to severe pain. Light, smells, sounds, movement can worsen the pain. Not everyone with migraine disease develops a headache.
experience the pain and disability of migraine, but many of them go undiagnosed or misdiagnosed because their symptoms don’t seem like “typical” or “classic” migraine symptoms.
You might have migraine disease.
Vestibular Migraine
A nervous system problem that causes vertigo (dizziness) in people with a history of migraine
Abdominal Migraine
Stomach pain, nausea, vomiting. Most diagnosed in children, but the disease often evolves into the more common migraine headaches
Self-Diagnosed Sinus Headache
Forehead/facial pressure, runny
nose/nasal congestion. Nearly always migraine (90% of the time3)
Migraine That Mimics Fibromyalgia (A condition marked by chronic pain)
Fatigue, chronic all-over body pain, severe headaches
Speak with your health care provider to learn about preventing or decreasing migraine symptoms using SEEDS for Success.4
Use your bedroom as a cue for sleep
Dark and cool room, quiet ± white noise machine, no screen (TV, phone, tablets)
Sleep
Exercise Eat
Diary
Stress
Planned bedtime and wake-up, no naps, get out of bed if not sleeping
Start exercising with a goal of 30–60 minutes 3–5 times a week
Start small and slowly increase exercise duration and frequency to make it a habit Choose an activity you enjoy since no one type of exercise is best
Eat healthy well-balanced meals at least 3 times a day; avoid skipping meals Stay hydrated, aiming for 7–8 glasses (8-oz) of water per day
Stop caffeine or consistently consume less than 1–2 cups of brewed coffee per day Aim for optimal weight
Track your headaches in a migraine diary — use a calendar, agenda or app Bring the diary to your follow-up for your doctor to review
Rescue medications should be used fewer than 2 days per week to avoid a rebound headache called “medication-overuse headache”
To help manage migraine, consider the following techniques:
Cognitive behavioral therapy, mindfulness, biofeedback, and relaxation techniques like visualization or progressive muscle relaxation
To learn more about migraine management, visit HealthyWomen.org. This resource was created with support from Allergan Foundation and Bausch Foundation.
- A New Device Can Help Healthcare Providers Treat Migraine Attacks ›
- Botox and Migraine: What You Need to Know ›
- Migraine Hub - HealthyWomen ›
- Can Migraine Attacks Be Triggered? - HealthyWomen ›
- A Perfect Storm Migraine Attack Revealed the Limits of My “Push Through the Pain” Philosophy - HealthyWomen ›
- Fact Facts: Everything You Need to Know About Migraine Disease - HealthyWomen ›
- Healing Environments Need to Recognize Migraine Triggers - HealthyWomen ›
- 8 tipos de migrañas - HealthyWomen ›
- I Finally Figured Out What Was Causing My Migraines - HealthyWomen ›
- Foods That Can Make Your Headaches Worse - HealthyWomen ›
- 8 Types of Migraines - HealthyWomen ›
- Migraine or Headache? Understanding the Difference - HealthyWomen ›