Editor's Note: As of April 3, 2020, the Centers for Disease Control and Prevention is recommending people wear cloth face coverings in public where social distancing measures may be difficult to maintain. Read more here.
By Thomas Perls, Boston University
As a professor at Boston University's School of Medicine and a geriatrician at Boston Medical Center caring for the most vulnerable in this pandemic, I've been asked a lot of questions about COVID-19.
It turns out there is good science out there that helps us know what masks we need to wear and when to wear them. That being said, some of the following advice could change as scientists learn more about why some people get a bad or even lethal case of this virus while many more get through it OK. One of the areas of greatest confusion seems to be about masks.
Much of the decision about wearing masks depends on what the essential businesses that remain open are doing to ensure social distancing and therefore, our safety.
Knowledge will protect you
Guidance about wearing a mask has to do with the different ways viruses like COVID-19 spread from person to person: through contact, droplets and as airborne, also called aerosolized, particles.
People get infected with COVID-19 when they touch a contaminated surface like a subway handle, or shake hands and then touch their face. Steel and plastic surfaces can harbor live virus for three days. On average, people touch their faces every two-and-a-half minutes, so it is easy to see how this virus can spread so easily from one person to the next by touching surfaces.
Another way to get the virus is by droplets that people produce by coughing and sneezing. Droplets are relatively large and contain mostly water plus the virus, so they usually fall from the air within six feet (one of the reasons for the six-foot social distancing rule). That said, vigorous coughs can go farther, and a strong sneeze – they've been clocked at 50-100 meters per second – can spread a droplet 18 feet away. This is why people who aren't already wearing a mask because they are sick should cough or sneeze into their elbow.
Coughs and sneezes also produce aerosolized virus, smaller particles that float in the air far longer than droplets and that can also travel farther. Aerosols are also produced by talking, yelling and just normal breathing. A big problem is that in small, poorly ventilated rooms, COVID-19 can hang in the air and stay infectious for three hours. Another thing to know is that common medical devices, like nebulizer machines for people with asthma and CPAP machines for those with sleep apnea, are good at aerosolizing virus.
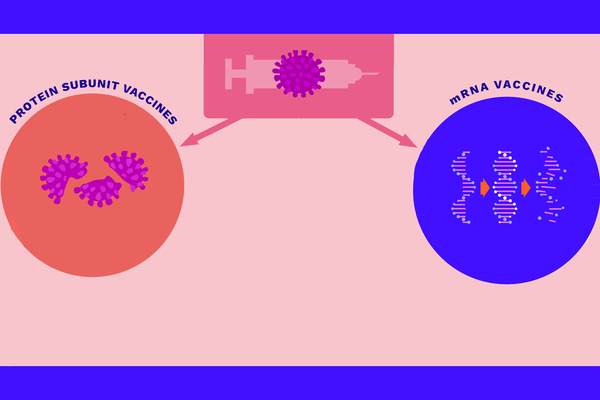
Two different types of masks to choose from
There are two basic kinds of masks – surgical masks and N95 respirator masks.
Surgical masks are worn to protect patients from infectious droplets should the health care provider sneeze or cough. Someone who is suspected of being sick or is actually sick with COVID-19 should also wear a surgical mask to protect anyone around them from their sneeze or cough.
As far as protection for the user, surgical masks can protect the nose and mouth against splashes of bodily fluids, as a surgeon might encounter during a surgery. But don't wear a surgical mask or a do-it-yourself mask if you think it's going to protect you from COVID-19 that's suspended in the air, say in a closed, poorly ventilated space. Aerosolized COVID-19 is so tiny that it can get in through gaps between the mask and face and breathed in through the material of the mask.
Some countries are requiring everyone to wear a surgical mask at least in potentially high people density, closed spaces. For example, the Austrian government now requires supermarkets and pharmacies to hand out surgical masks to all customers who must wear them when in the store. The purpose of the masks is to prevent the wearer from spreading the virus to others by coughing and sneezing. If markets and other businesses and our means of transportation can't enforce good social distancing and even just some people who are coughing or sneezing don't wear masks when they venture out, then the United States and other countries might have to follow suit.
Several U.S. government officials have suggested that widespread public use of masks will help. FDA Commissioner Gottlieb argued that a mask can be “an additional layer of protection for those who have to go out.” To be clear though, surgical or DIY masks and scarves are used primarily to protect others by preventing the spread of droplets. People should not be lulled into a false sense of security in thinking that these types of masks will protect them from airborne, aerosolized virus in for example, poorly ventilated spaces frequented by others. The best thing to do is avoid such spaces and stay home as much as possible.
A N95 respirator mask (in Europe, it's called a FFP2) does protect the wearer from breathing in COVID-19 if it's worn properly so that there is a really good seal around the face. If you're a home care provider caring for someone who has or might have COVID-19, you should wear the N95 to protect yourself. That is, assuming there are enough of these masks to go around beyond those needed by care providers on the front lines at the hospitals. If you don't have a N95, open a window in the patient's room and maybe even use a fan if you have one to decrease the amount of virus floating around. Of course provide plenty of blankets to keep them warm!
The bottom line
In my opinion, you don't need a mask with really good social distancing (staying at least six feet away from others) when you are outdoors. Even in a well-ventilated, large room where businesses are doing a good job of keeping the density of people small and you are there for as short a time as possible, I would not feel the need for a mask. But if those who are sneezing or coughing are not wearing masks and if social distancing doesn't seem to be slowing the spread of COVID-19 fast enough, Americans and others will likely need to follow in Austria's footsteps with mandatory masks inside buildings and go further to include any public transportation, taxis and ride sharing services.
If you are coughing or sneezing and therefore producing droplets that can contaminate other people or surfaces, wear a surgical mask to protect others. Even if you think it's just a cold, wear a mask, or if you don't have one, then a scarf. Pretty soon we may all be asked to wear these when we go to public places even if we aren't coughing or sneezing, if some people don't take this responsibility very seriously.
A N95 mask should be worn by people caring for COVID-19-suspected or infected people which, when worn properly, can protect against airborne virus. Because health care professionals are caring for many COVID-19 patients, they must have N95 masks. If there are enough, then asymptomatic caregivers of COVID-19 patients at home should also wear them.
Thomas Perls, Professor of Medicine, Boston University
This article is republished from The Conversation under a Creative Commons license. Read the original article.