By Mindy Aisen, University of Southern California
For COVID-19, like all illnesses, the drugs and vaccines to treat or prevent the disease must be backed by rigorous evidence. Clinical trials are the source of this evidence.
With vaccines and drugs for the coronavirus already entering human testing, it is important to know what the different phases of clinical trials are testing for. I am a neurologist with the Alzheimer’s Therapeutic Research Institute at the University of Southern California. Our team has been developing and overseeing all phases of clinical trials for decades. I am here to help you understand this complicated and important process.
Preclinical trials
The earliest indications about whether an intervention is effective and safe come from preclinical trials. This research is done in the laboratory using cells or animals.
Researchers can get some information about safety and efficacy of a treatment from preclinical trials, but the results do not say whether what they are testing is safe or works in people.
Once a treatment shows promise in preclinical trials, researchers begin the process of working through the phases that have been established by the U.S. Food and Drug Administration. These phases are designed to do two things: protect patients during the process and make sure that the drug or treatment works.
Phase 1 trials
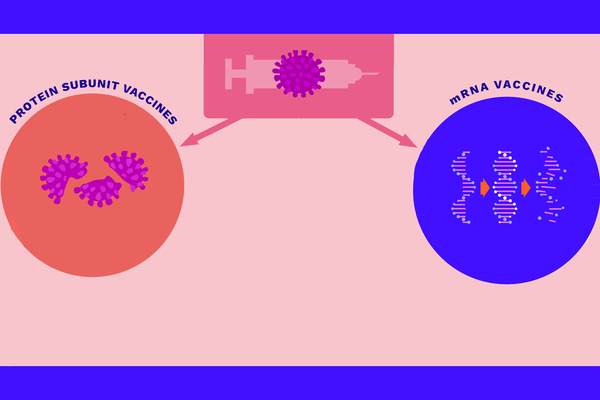
Phase 1 trials are focused on safety. Researchers monitor kidney, liver, hormone and cardiac functions to look for adverse affects in human volunteers. They also look for biological signs of efficacy related to what they are hoping to treat. For example, if a trial was testing a vaccine, researchers might monitor immune activity to see if it increases.
Phase 1 clinical trials typically take around two months and involve small numbers of participants, usually 20 to 100 healthy volunteers or people with the condition that the intervention may treat. Researchers give the participants a range of medication dosages to help determine the lowest possible effective but safe dose. Some, but not all, phase 1 studies are randomized and placebo controlled, meaning that some portion of the subjects are given the real treatment and some get a placebo that does nothing. Neither the subject nor clinician knows who is receiving which treatment.
Drugs that pass phase 1 trials can be considered likely safe, but whether they work or not still remains to be seen.
Phase 2 trials
In phase 2 trials, researchers focus on seeing if the treatment works, finding the safest effective dose and determining what symptoms, tests or outcomes are the best measures of efficacy of the treatment. Determining the best measures of success is important for designing the final stage of testing.
All phase 2 trials are randomized and placebo controlled.
This stage of research can take months to years, and only about one-third of drugs in phase 2 trials make it to the next phase.
In phase 2 trials, researchers give the drug to hundreds of subjects and watch for safety through regular testing. To measure effectiveness, researchers look at clinical responses such as the length of illness, severity of the illness or survival rates. Direct measures of a disease – such as the amount of virus in a person’s cells – are also monitored, as well as biomarkers – signals in the body that researchers know are changed by the targeted disease.
At this point, the researchers will use all the information they have gained to design the phase 3 trial. They decide what measures to use, the doses to test and the type, or cohort, of people to test.
If there is evidence in either phase 1 or phase 2 that the drug or vaccine is unsafe or ineffective, the teams will stop the trial.
Phase 3 trials
Phase 3 trials are where researchers look to see if people that get the treatment are statistically better off than those don’t. The trials are randomized and placebo controlled, and use the measures of success chosen from the phase 2 trial. Phase 3 trials are also designed to find any rare side effects of a treatment.
In order to get statistically meaningful data, phase 3 trials are big, normally including a few hundred to 3,000 people.
This is the final step before a drug is approved for public use. After a phase 3 trial is finished, the FDA puts together a panel of independent scientists to review the data. The panel decides, based on evidence of success and prevalence of side effects, if the benefits of the drug outweigh the risks enough to approve it for widespread use.
According to the FDA, only 25%-30% of drugs in phase 3 trials get approved.
Phase 4 trials
Phase 4 trials are used to test approved treatments for the same medical condition but in a different dose or time frame or group of people. For example, a phase 4 trial could be used to test if a drug that’s already approved for adults is safe and effective for children.
When a drug that’s been approved for one purpose is studied for a different medical condition – for example, testing the malaria drug hydroxychloroquine as a potential treatment for COVID-19 – this is not a phase 4 trial. This is a phase 2 or 3 trial because it is designed to answer those early questions about how well the treatment works for the new condition.
A critical eye for medical news
News headlines are full of trial results concerning COVID-19 interventions. It’s easy to get excited when reading about a new drug or vaccine. But early successes do not guarantee a treatment will work.
COVID-19, like Alzheimer’s, is a complex disease, and clinical trials to test treatments are particularly challenging, with highly variable outcomes. The process for drug and treatment approval is long, but is designed to guarantee that what a physician gives you will do help, not hurt, you.
Mindy Aisen, Clinical Professor of Neurology, University of Southern California
This article is republished from The Conversation under a Creative Commons license. Read the original article.