By Ryan Malosh, University of Michigan
Editor's note: Now that states are relaxing social distancing restrictions, people desperately want to see friends and family, go to a restaurant and let our kids have play dates. Even grocery shopping sounds fun. But how can you do that and still stay safe? Here, an epidemiologist who is immune-compromised himself, walks you through some decision making.
The Centers for Disease Control and Prevention (CDC) has finally released new guidelines for businesses, bars and schools that are considering reopening. Although following these guidelines should help, it's frustrating there hasn't been more clear, concise communication about the risk of infection. And without strict guidelines, it will be up to us to minimize our own risk and the risk of everyone around us.
In large part, this is because there is still so much we scientists and physicians don't know about the new coronavirus. The pace of new research on the virus, SARS-CoV-2, and the disease it causes, COVID-19, is truly astonishing. There are also times when the science and the necessity of the moment are in conflict; a prime example is the confusion about using face masks while a worldwide shortage of personal protective equipment exists.
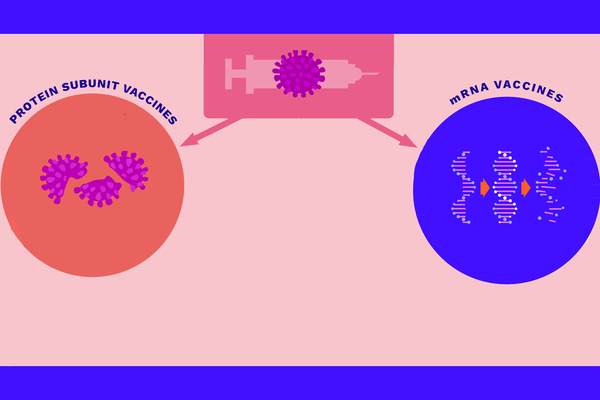
And the pattern of disease is extremely localized. Michigan's outbreak looks different from Iowa's, which looks different from Colorado's. Even within states, outbreaks are very distinct. The outbreak I'm experiencing in southeast Michigan is not like the one my grandparents are experiencing two hours north of here. As a research scientist, I study herd immunity and vaccine effectiveness. As we slowly begin to return to normal life – albeit a new normal – I can tell you there are ways we can minimize our risk.
As a survivor of leukemia and a bone marrow transplant, I am part of a high-risk population, so my risk calculation is likely different from yours. As my state starts to relax restrictions, I will continue to limit my interactions with others as much as I can. Here are things you can consider.
What's associated with a high risk of transmission?
How SARS-CoV-2 transmits from person to person is still a mystery. It can certainly be transmitted by large respiratory droplets, like those produced when we cough or sneeze. Evidence also suggests that smaller aerosol particles, spread while talking or breathing, can lead to transmission. There is some evidence that people can transmit the virus before they have symptoms, although they will likely have the highest amount of virus close to the start of the illness.
Taking all this together, it's safe to say the riskiest thing you can do is to come into close contact with sick people. That's why the advice about self-isolation if you feel ill is so important.
It's also becoming clear the virus transmits most effectively in indoor settings. There, close contact between infected people and inadequate ventilation are more likely. The infection risk is especially high among household contacts. Efficient transmission in crowded, enclosed spaces also explains the high attack rates in nursing homes, food processing plants, jails and prisons and cruise ships. On the flip side, the risk of transmission does seem to be lower outdoors.
How do we minimize risk?
If the riskiest thing is to be in a crowd while indoors with sick people, then it follows the least risky behavior is to be in small groups, outdoors and to avoid sick people.
I think it will help to describe a simple model of infectious disease. The rate of new infections over a given time period is called the “force of infection,” which depends on a few things: the rate at which people contact each other; the probability of infection given contact; and the number of infectious individuals in a population.
This means our ability to prevent new infections depends on two things: reducing the rate at which people contact each other – or reducing the probability of infection given contact.
Reducing the contact rate was the goal of stay-at-home measures. By all accounts, this is still the most effective tool to prevent new infections.
Other non-pharmaceutical interventions, like facemasks and hand-hygiene, reduce the effective contact, or the chance the virus is transmitted if there is contact. Universal masking may be particularly effective if we can't rely on symptomatic screening for identifying infectious cases.
Or maybe you've heard of the layers of swiss cheese. Sometimes you have a few interventions (slices of Swiss cheese), but none are perfect (the holes). But stack the slices up, and the holes start to cover up. Layering imperfect interventions can, in a similar way, slow down transmission.
So what does it all mean?
I once read a quote about the common cold from Ian Mackay, an Australian virologist: “The only fail-safe means of avoiding a cold is to live in complete isolation from the rest of humanity.” The same is probably true for COVID-19.
But that's not realistic. Authorities should borrow ideas from HIV prevention, and focus on clear messages for harm reduction. In the absence of stay-at-home orders, all of us will have to decide for ourselves how much risk we are willing to tolerate.
I'm a leukemia survivor, so I will factor that in. You, too, will need to consider your medical history. When I'm not in isolation, I will stack as many layers of swiss cheese as I can to minimize any risk: staying 6-10 feet away from others, wearing masks, staying outdoors.
I think these are generally common sense guidelines for anyone.
- If your local authorities allow small gatherings, then getting together with friends who aren't sick or who haven't been in contact with other sick people is safest outdoors.
- Try to stay as far apart from each other as you can.
- Keep a mask and hand sanitizer nearby.
- Don't share food or drinks.
- If anyone feels sick or has had recent contact with someone who feels sick they should skip the playdate (this goes for adults and kids).
- If you are seeing someone at high risk of severe disease, an older relative or someone with a compromised immune system, take even more precautions and consider whether you can connect with them virtually.
Ryan Malosh, Assistant Research Scientist, University of Michigan
This article is republished from The Conversation under a Creative Commons license. Read the original article.