Cervical cancer is rare in the U.S. — making up less than 1% of all cancers — and it’s highly treatable. In fact, if it’s found in early stages, the 5-year survival rate is over 91%.
“Cervical cancer in the United States should be preventable. We've got an excellent screening test, with Pap smears and HPV testing,” said Monica Vetter, M.D., a board-certified gynecologic oncologist with Norton Cancer Institute.
Even though routine screening can prevent almost all cervical cancers, nearly 1 out of 4 women were overdue for their cervical cancer screenings in 2019. And it was estimated that more than 13,800 people were diagnosed with cervical cancer in 2024.
Asian women, Hispanic women and women living in rural areas were more likely to be behind on their screenings. And a 2022 study found that 1 in 4 Hispanic and Black women have delayed follow-ups, with Black women having the lowest follow-up rates after abnormal findings. Black women are also more likely to have higher rates of cervical cancer, more advanced stages at diagnosis and higher mortality.
Members of the LGBTQ community are also more likely to be behind on screening and are more likely to be incorrectly told by a healthcare provider that they do not need cervical cancer screening.
Read: Removing Barriers to Cervical Cancer Screening for the LGBTQ Community >>
Treatment for cervical cancer
If you have cervical cancer, you’ll likely be referred to a gynecologic oncologist, a doctor that specializes in treatment for cancer of the female reproductive system. Treatment can include surgery, chemotherapy, radiation, targeted therapy and immunotherapy. Which treatment is best for you depends on several factors, including the cancer stage and whether you want to get pregnant in the future.
Surgery
Surgery, along with some other treatments, can affect your ability to get pregnant in the future. Fertility-sparing surgeries, conization or radical trachelectomy, are options for early-stage cervical cancer.
Cone biopsy
Cone biopsy, also called conization, is a surgical option for precancerous cells and early-stage cervical cancer that will still allow you to potentially get pregnant. A cone biopsy takes a large amount of tissue and can also get rid of abnormal cells so they don’t become cancer in the future. “I tell people to think about it like I’m trying to take an ice cream scoop out of the center of their cervix,” Vetter said
There are three types of cone biopsies:
- Cold knife cone biopsy, which uses a surgical blade
- Laser conization, which uses a laser beam
- Loop electrosurgical excision procedure (LEEP), LEEP which uses a heated metal loop to scoop out cervical tissue for biopsy.
LEEPs can be done in the office using local anesthesia, whereas cone biopsies happen in the operating room, likely under general anesthesia.
Radical trachelectomy
Depending on the size and features of your cancer, your surgeon may recommend a trachelectomy instead of conization. A simple trachelectomy removes just the cervix and a radical trachelectomy removes the cervix and surrounding tissue. Your surgeon may also recommend the removal of nearby lymph nodes. Trachelectomies allow for the possibility of future pregnancy because the uterus is left in place. These procedures are done in an operating room under general anesthesia.
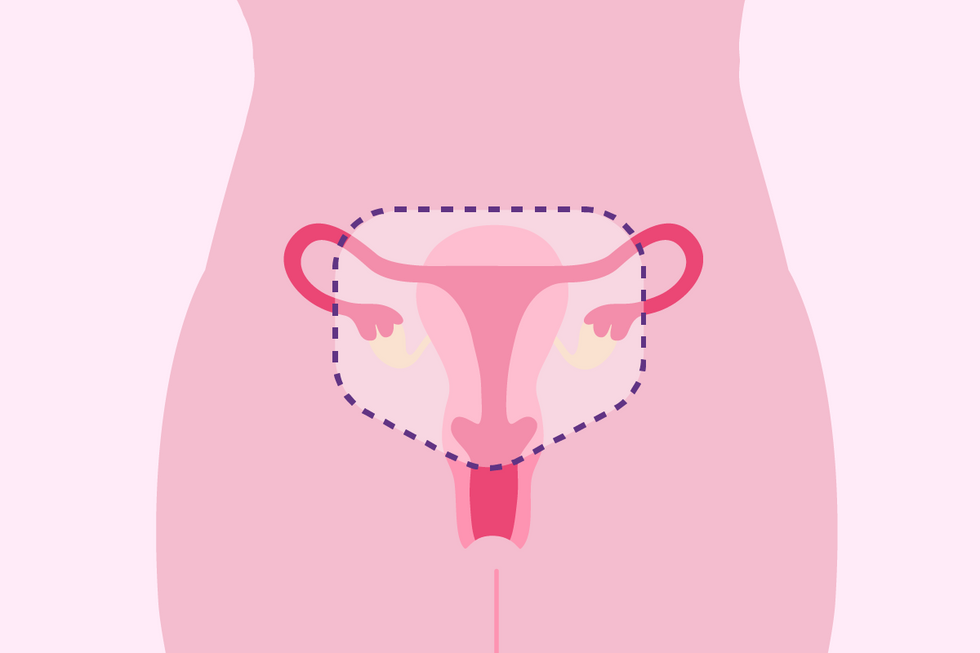
Hysterectomy
There are several types of hysterectomies that can be used to treat cervical cancer. All of them remove the option of getting pregnant in the future.
In a total or simple hysterectomy, the surgeon removes the uterus, including the cervix. The ovaries are usually left in place. This type of hysterectomy can be used to treat certain types of very early cervical cancer.
Radical hysterectomies are a more complicated surgery that removes the uterus and cervix as well as the tissue surrounding the cervix and the upper part of the vagina. The ovaries usually are not removed. Radical hysterectomies have more potential side effects than total hysterectomies, such as bowel or bladder complications.
Hysterectomies can be performed through the abdomen or vagina, and can be open surgery or minimally invasive surgery, including laparoscopic or robotic-assisted surgery. Depending on the stage of your cervical cancer, your surgeon may recommend open surgery as the safest option for hysterectomy. Your surgeon will be able to explain the risks and benefits of the different routes of hysterectomy in your case.
Chemotherapy, radiation and drug therapies

Chemotherapy is a treatment that uses drugs to kill or slow the growth of cancer cells. It is usually given via IV infusions.
Radiation therapy uses high energy X-rays to kill cancer. Radiation can be administered with X-ray machines, called external beam radiation, or with small capsules that are placed near or in the cervix, called internal or implant radiation.
Radiation is commonly given in combination with chemotherapy, known as chemo-radiation, because it’s more effective than radiation alone. Chemotherapy and/or radiation are sometimes used after hysterectomy and chemo-radiation can be used for tumors that are too big for a hysterectomy. Sometimes chemo-radiation is curative.
Chemotherapy alone is often given if you can’t do other treatments or if you have recurrent cervical cancer — cancer that’s come back after being treated by surgery or chemo-radiation. Unfortunately, it’s not possible to become pregnant after you’ve had chemo-radiation therapy because of the radiation damage to the uterus.Immunotherapy
Immunotherapy uses your body’s immune system to fight cancer and is often used along with chemotherapy, particularly if you have stage 4 cancer at diagnosis. Given by IV infusion, immunotherapy works by taking away the cancer’s ability to hide from immune cells and improving your immune system’s ability to destroy the cells. Not everyone is a candidate for immunotherapy, but if you are and can get the therapy to respond to the cancer, it can keep you in remission longer. Your ability to conceive after immunotherapy will depend on the type of treatment you had. Some treatments interfere with your fertility and others carry a high chance of causing birth defects.
Targeted drug therapy
Targeted drug therapy uses medicine that blocks proteins that help cancer cells grow and spread. Some targeted drug therapies are IV infusions and some are pills. Some targeted therapies are also considered immunotherapy.
Targeted drug therapy is often used for recurrent disease. More research is needed to fully understand how targeted drug therapy affects fertility.Screening is key
“The incidence or the rate of advanced-stage cancers is increasing, and we need to do a better job of getting people screened,” Vetter said. “Get your Pap [tests]. If you're having any weird symptoms, like vaginal bleeding after sex or bleeding in between periods, go in and be evaluated. When cervical cancer is caught early, there’s a very high cure rate.”
This educational resource was created with support from Merck.
- Why Are More Women Being Diagnosed with Cervical Cancer Later? ›
- True or False: Cervical Cancer ›
- Living with Cervical Cancer ›
- Pregnancy and Cervical Cancer: Know Your Options ›
- Cervical Cancer Screening Is Essential, but Access to Good Treatment Can Be the Difference Between Life and Death ›
- Cervical Cancer Stages and Treatments ›