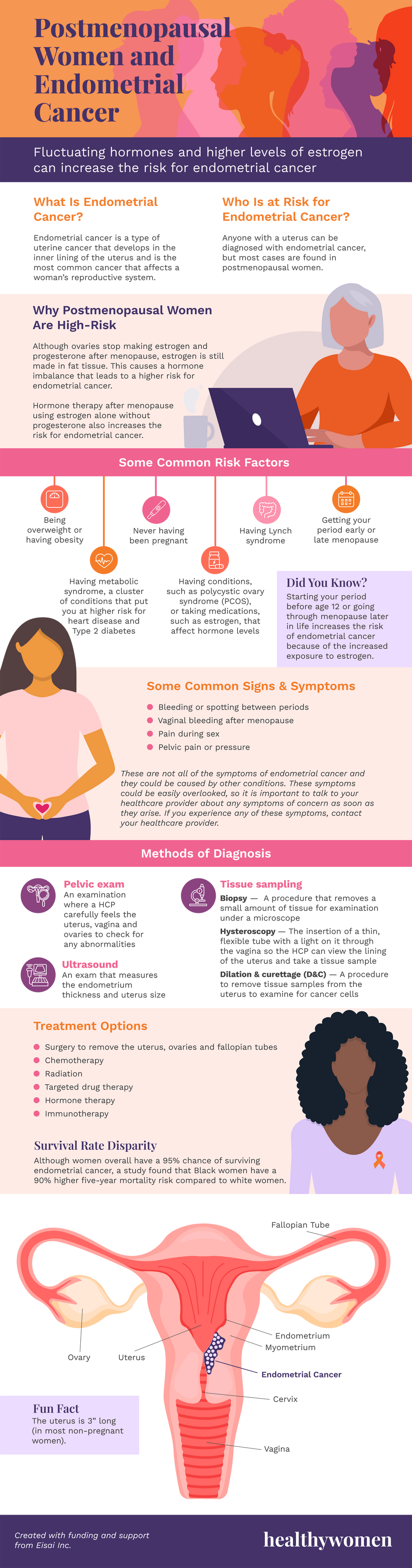
Postmenopausal Women and Endometrial Cancer
Fluctuating hormones and higher levels of estrogen can increase the risk for endometrial cancer
What Is Endometrial Cancer?
Endometrial cancer is a type of uterine cancer that develops in the inner lining of the uterus and is the most common cancer that affects a woman’s reproductive system.
Who Is at Risk for Endometrial Cancer?
Anyone with a uterus can be diagnosed with endometrial cancer, but most cases are found in postmenopausal women.
Why Postmenopausal Women Are High-Risk
Although ovaries stop making estrogen and progesterone after menopause, estrogen is still made in fat tissue. This causes a hormone imbalance that leads to a higher risk for endometrial cancer.
Hormone therapy after menopause using estrogen alone without progesterone also increases the risk for endometrial cancer.
Some Common Risk Factors
- Getting your period early or late menopause
- Being overweight or having obesity
- Having metabolic syndrome, a cluster of conditions that put you at higher risk for heart disease and Type 2 diabetes
- Having conditions, such as polycystic ovary syndrome (PCOS), or taking medications, such as estrogen, that affect hormone levels
- Never having been pregnant
- Having Lynch syndrome
Did You Know?
Starting your period before age 12 or going through menopause later in life increases the risk of endometrial cancer because of the increased exposure to estrogen.
Some Common Signs & Symptoms
- Bleeding or spotting between periods
- Vaginal bleeding after menopause
- Pain during sex
- Pelvic pain or pressure
These are not all of the symptoms of endometrial cancer and they could be caused by other conditions. These symptoms could be easily overlooked, so it is important to talk to your healthcare provider about any symptoms of concern as soon as they arise. If you experience any of these symptoms, contact your healthcare provider.
Methods of Diagnosis
- Pelvic exam — An examination where a HCP carefully feels the uterus, vagina and ovaries to check for any abnormalities
- Ultrasound — An exam that measures the endometrium thickness and uterus size
- Tissue sampling —
- Biopsy — A procedure that removes a small amount of tissue for examination under a microscope
- Hysteroscopy — The insertion of a thin, flexible tube with a light on it through the vagina so the HCP can view the lining of the uterus and take a tissue sample
- Dilation & curettage (D&C) — A procedure to remove tissue samples from the uterus to examine for cancer cells
Treatment Options
- Surgery to remove the uterus, ovaries and fallopian tubes
- Chemotherapy
- Radiation
- Targeted drug therapy
- Hormone therapy
- Immunotherapy
Survival Rate Disparity
Although women overall have a 95% chance of surviving endometrial cancer , a study found that Black women have a 90% higher five-year mortality risk compared to white women.
Anatomy of the Uterus
Fun Fact
The uterus is 3” long (in most non-pregnant women).
This resource was created with funding and support from Eisai Inc.
References
https://www.britannica.com/science/human-reproductive-system/The-uterus
https://www.cancer.org/cancer/endometrial-cancer/causes-risks-prevention/risk-factors.html
https://www.cancer.org/cancer/endometrial-cancer/detection-diagnosis-staging/signs-and-symptoms.html
https://www.cancer.org/cancer/endometrial-cancer/detection-diagnosis-staging/how-diagnosed.html
https://www.cancer.org/cancer/endometrial-cancer/treating.html
https://www.mayoclinic.org/diseases-conditions/endometrial-cancer/symptoms-causes/syc-20352461
https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
- Fast Facts: What You Need to Know About Endometrial Cancer ›
- Clinically Speaking: Questions to Ask Your HCP About Endometrial Cancer ›
- How Endometrial Cancer Is Diagnosed - HealthyWomen ›
- Ask the Expert: Endometrial Cancer - HealthyWomen ›
- My Endometrial Cancer Hid in Menopause - HealthyWomen ›
- Metabolic Syndrome and Endometrial Cancer: What’s the Connection? - HealthyWomen ›
- Doctors Overlooked My Endometrial Cancer Symptoms - HealthyWomen ›