Designed by Sarah Hoctor
Janelle Scales, 37, an anti-bias consultant based in the Los Angeles area, runs a firm helping others diminish bias. But she blames her own internalized ableism — bias against people who are not able-bodied — for not getting the support she needed to manage her asthma sooner.
Scales says she couldn’t walk more than a quarter of a mile without needing her rescue inhaler, a fast-acting medicine used to open airways that narrow during an asthma attack.
Even with her rescue inhaler, Scales needed urgent care multiple times a year and lost sleep many nights, waking up unable to breathe. Lacking energy, Scales felt she couldn’t offer her daughters her best. She even had to avoid watching comedies because laughing triggered asthma attacks.
“Honestly, just recounting the hardships of life before having my asthma under control makes me shudder,” Scales said.
According to Scales, the first step to getting her asthma under control was finding the right doctor. That doctor recommended Scales see an ear, nose and throat specialist and undergo allergy testing to find out exactly what was triggering her asthma. It turned out Scales is allergic to pretty much everything: cats, dogs, horses, pollen, grass, dust and mold, among others.
Now, Scales follows a basic treatment plan with daily medications and consistent care. Her routine includes allergy shots and pills, nasal steroids and inhaled steroids.
Sticking to this treatment plan has been working for around a year. She can run several times a week, which enhances her mood, and fully engage in her work and as a parent educator for her homeschooled children.
“Having my asthma under control gives me the ability to live life on my own terms,” Scales said.
Asthma in women
Scales is one of nearly 13 million women in the United States with asthma. Not only are adult women nearly twice as likely as adult men to have asthma but women also tend to experience more severe asthma than their male counterparts.
A 2015 review article suggested sex hormones could explain these differences, but a later study showed that estrogen and progesterone do not actually seem to increase women’s asthma risks. Instead, it’s the other way around: Testosterone appears to protect men from asthma and severe symptoms.
“Asthma can wax and wane in life, starting in childhood,” said Dr. Neeta Ogden, director of the Allergy, Asthma and Sinus Center in Edison, New Jersey. “It may look different for women — it can get worse in pregnancy or in hormonal changes like menopause, especially if there is weight gain, which can also put further burden on breathing.”
Asthma signs and symptoms can vary from person to person
Asthma can look different in different people. For example, wheezing and difficulty breathing after exercise are common in children with asthma, while older adults may experience more coughing that produces fluid. Asthma symptoms in older people may be confused for bronchitis, emphysema or congestive heart failure.
Signs and symptoms
- Shortness of breath
- Whistling sounds when you breathe
- Coughing, wheezing
- Poor sleep as a result of symptoms
- Tightness or pain in your chest
- Asthma symptoms when you exercise
- Sneezing and runny nose
- Changes to the phlegm you cough up
Symptoms might be triggered by exercise, cold weather, air pollution or respiratory illnesses.
Recognizing your specific asthma triggers, monitoring and working to improve your indoor air quality, following up regularly with your healthcare provider especially before seasonal or other triggers, and making sure you have medication refills are all strategies that Ogden said can help you make your asthma manageable.
Treating asthma
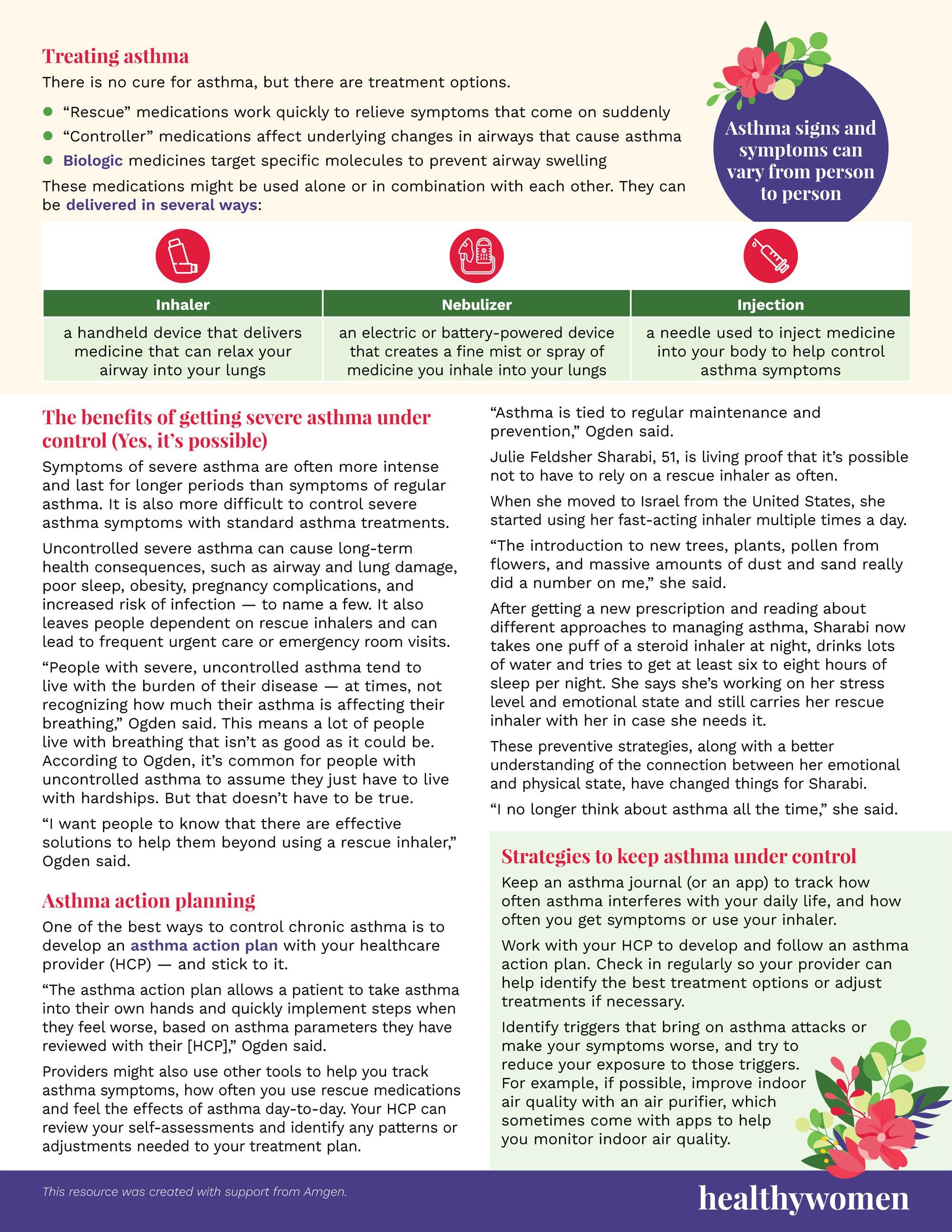
There is no cure for asthma, but there are treatment options.
- “Rescue” medications work quickly to relieve symptoms that come on suddenly
- “Controller” medications affect underlying changes in airways that cause asthma
- Biologic medicines target specific molecules to prevent airway swelling
These medications might be used alone or in combination with each other. They can be delivered in several ways:
- Inhaler — a handheld device that delivers medicine that can relax your airway into your lungs
- Nebulizer —an electric or battery-powered device that creates a fine mist or spray of medicine you inhale into your lungs
- Injection — a needle used to inject medicine into your body to help control asthma symptoms
The benefits of getting severe asthma under control (Yes, it’s possible)
Symptoms of severe asthma are often more intense and last for longer periods than symptoms of regular asthma. It is also more difficult to control severe asthma symptoms with standard asthma treatments.
Uncontrolled severe asthma can cause long-term health consequences, such as airway and lung damage, poor sleep, obesity, pregnancy complications, and increased risk of infection — to name a few. It also leaves people dependent on rescue inhalers and can lead to frequent urgent care or emergency room visits.
“People with severe, uncontrolled asthma tend to live with the burden of their disease — at times, not recognizing how much their asthma is affecting their breathing,” Ogden said. This means a lot of people live with breathing that isn’t as good as it could be. According to Ogden, it’s common for people with uncontrolled asthma to assume they just have to live with hardships. But that doesn’t have to be true.
“I want people to know that there are effective solutions to help them beyond using a rescue inhaler,” Ogden said.
Asthma action planning
One of the best ways to control chronic asthma is to develop an asthma action plan with your healthcare provider (HCP) — and stick to it.
“The asthma action plan allows a patient to take asthma into their own hands and quickly implement steps when they feel worse, based on asthma parameters they have reviewed with their [HCP],” Ogden said.
Providers might also use other tools to help you track asthma symptoms, how often you use rescue medications and feel the effects of asthma day-to-day. Your HCP can review your self-assessments and identify any patterns or adjustments needed to your treatment plan.
“Asthma is tied to regular maintenance and prevention,” Ogden said.
Julie Feldsher Sharabi, 51, is living proof that it’s possible not to have to rely on a rescue inhaler as often.
When she moved to Israel from the United States, she started using her fast-acting inhaler multiple times a day.
“The introduction to new trees, plants, pollen from flowers, and massive amounts of dust and sand really did a number on me,” she said.
After getting a new prescription and reading about different approaches to managing asthma, Sharabi now takes one puff of a steroid inhaler at night, drinks lots of water and tries to get at least six to eight hours of sleep per night. She says she’s working on her stress level and emotional state and still carries her rescue inhaler with her in case she needs it.
These preventive strategies, along with a better understanding of the connection between her emotional and physical state, have changed things for Sharabi.
“I no longer think about asthma all the time,” she said.
Strategies to keep asthma under control
- Keep an asthma journal (or an app) to track how often asthma interferes with your daily life, and how often you get symptoms or use your inhaler.
- Work with your HCP to develop and follow an asthma action plan. Check in regularly so your provider can help identify the best treatment options or adjust treatments if necessary.
- Identify triggers that bring on asthma attacks or make your symptoms worse, and try to reduce your exposure to those triggers. For example, if possible, improve indoor air quality with an air purifier, which sometimes come with apps to help you monitor indoor air quality.
This resource was created with support from Amgen.