Designed by Megan Schofield
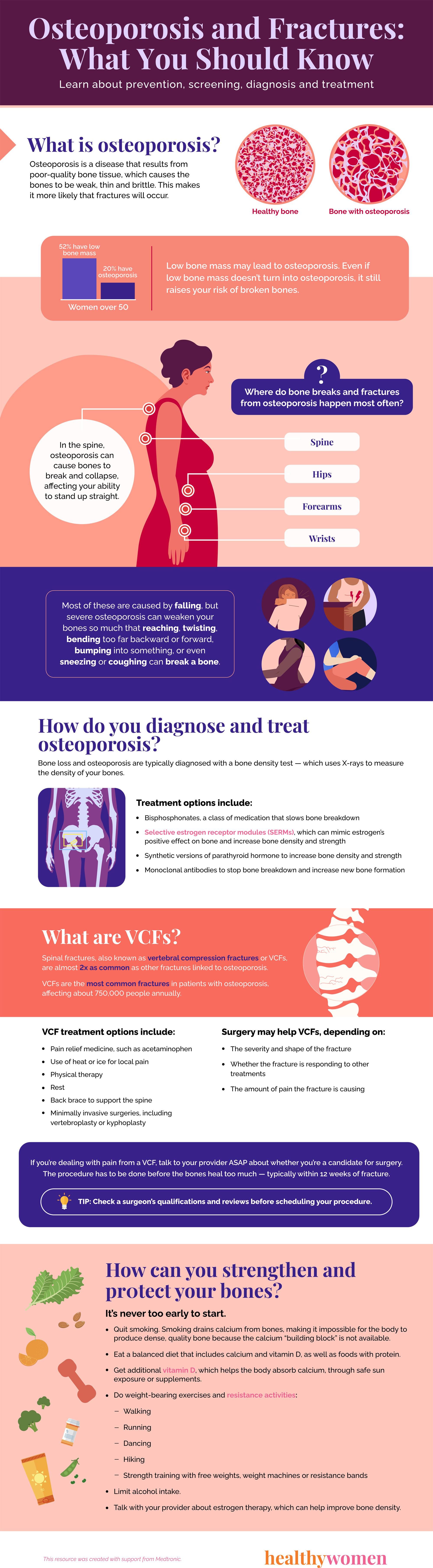
What is osteoporosis?
Osteoporosis is a disease that results from poor-quality bone tissue, which causes the bones to be weak, thin and brittle. This makes it more likely that fractures will occur.
Images:
Healthy bone
Bone with osteoporosis
About 20% of women over 50 have osteoporosis, and 52% have low bone mass.
- Low bone mass may lead to osteoporosis. Even if low bone mass doesn’t turn into osteoporosis, it still raises your risk of broken bones.
Where do bone breaks and fractures from osteoporosis happen most often?
- Spine
- Hips
- Wrists
- Forearms
Most of these are caused by falling, but severe osteoporosis can weaken your bones so much that reaching, twisting, bending too far backward or forward, bumping into something, or even sneezing or coughing can break a bone.
In the spine, osteoporosis can cause bones to break and collapse, affecting your ability to stand up straight.
How do you diagnose and treat osteoporosis?
Bone loss and osteoporosis are typically diagnosed with a bone density test — which uses X-rays to measure the density of your bones.
Treatment options include:
- Bisphosphonates, a class of medication that slows bone breakdown
- Selective estrogen receptor modules (SERMs), which can mimic estrogen’s positive effect on bone and increase bone density and strength
- Synthetic versions of parathyroid hormone to increase bone density and strength
- Monoclonal antibodies to stop bone breakdown and increase new bone formation
How can you prevent osteoporosis?
It’s never too early to start strengthening and protecting your bones.
- Quit smoking. Smoking drains calcium from bones, making it impossible for the body to produce dense, quality bone because the calcium “building block” is not available.
- Eat a balanced diet that includes calcium and vitamin D, as well as foods with protein.
- Get additional vitamin D, which helps the body absorb calcium, through safe sun exposure or supplements.
- Do weight-bearing exercises and resistance activities:
- Walking
- Running
- Dancing
- Hiking
- Strength training with free weights, weight machines or resistance bands
- Limit alcohol intake.
- Talk with your provider about estrogen therapy, which can help improve bone density.
What are VCFs?
Spinal fractures, also known as vertebral compression fractures or VCFs, are almost 2x as common as other fractures linked to osteoporosis.
VCFs are the most common fractures in patients with osteoporosis, affecting about 750,000 people annually.
VCF treatment options include:
- Pain relief medicine, such as acetaminophen
- Use of heat or ice for local pain
- Physical therapy
- Rest
- Back brace to support the spine
- Minimally invasive surgeries, including vertebroplasty or kyphoplasty
Surgery may be used to treat VCFs, depending on:
- The severity and shape of the fracture
- Whether the fracture is responding to other treatments
- The amount of pain the fracture is causing
If you’re dealing with pain from a VCF, talk to your provider ASAP about whether you’re a candidate for surgery. The procedure has to be done before the bones heal too much — typically within 12 weeks of fracture.
- TIP: Check a surgeon’s qualifications and reviews before scheduling your procedure.
This resource was created with support from Medtronic.
- Clinically Speaking: Questions to Ask Your Healthcare Provider ... ›
- Staying Fracture-Free - HealthyWomen ›
- How is Osteoporosis Diagnosed - HealthyWomen ›
- What is Osteoporosis - HealthyWomen ›
- Women and Bone Health Basics - HealthyWomen ›
- 7 Ways to Prevent Bone Loss - HealthyWomen ›
- What You Need to Know About Osteoporosis - HealthyWomen ›
- My Back Pain Was a Vertebral Compression Fracture - HealthyWomen ›