by Dr. Anita Gupta
Why Does Communication Matter to Doctors and Patients Before and After Surgery?
Hospitalization and surgery are demanding life events that lead to considerable stress and anxiety in patients. The fear of the "unknown" is a powerful force for the patient especially during the perioperative surgical time period. Unfortunately, medical errors and medications errors are often linked to miscommunication, anxiety and poor patient satisfaction which are common occurrences. Moreover, patients perceive the day of surgery as one of the most intimidating days in their lives and there is a real absence of information on predictors of anxiety in the current literature. Additionally, there is mounting evidence that patient education is one critical way to combat stress and anxiety during this time period. Studies have shown that preoperative surgical education can significantly reduce stress and anxiety preoperatively, therefore increasing patient satisfaction.
Preoperative patient education, particularly in regards to medications, is also an essential component of patient safety and satisfaction in today's healthcare arena. It's been suggested that changes in preoperative patient education, particularly in a pre-admission assessment testing unit (PATs), is an excellent starting point for an improvement in patient safety and for the increase in satisfaction ratings.
Framing the Response in a Philadelphia Hospital
The hospital where this project was implemented was at a for-profit, minimally resourced university teaching hospital in Philadelphia, PA. Moreover, high risk populations, such as substance use disorders, combined with hospitals that are have low access to adequate resources in busy overpopulated urban centers, such as in Philadelphia, pose further burdens on the providers taking care of these patients during surgery. Adding to this is the mounting pressures of productivity, checklists, and efficiency, create minimal time for adequate shared-decision making for communication during the surgical process.
At the time, when I joined the anesthesiology department, there was no organizational health system infrastructure for a pain service or handling a mounting opioid crisis or a broad systemic, pre-operative consultation service to address patient questions immediately prior to surgery. Many patients would only be requested to visit a routine testing center with minimal guidance on how much pain they would have and the risks involved during the course of surgery. Moreover, the high-risk patients that had opioid pain medications or a history of substance use disorders (which was highly prevalent in this population) prior to surgery were less likely to be appropriately screened prior to surgery and less likely to have follow up afterwards since no high-risk clinic existed within the health system. In order to streamline the process, I was charged to organize these processes before, during and after surgery to ensure these high-risk patients had improved pain and communication and ultimately overall better patient satisfaction.
In order to streamline the process, I wanted to first improve communication with patients with an established tool that was standardized. I was already engaged with the World Health Organization (WHO) on prior work regarding pain and was familiar with tools they used for pain and surgery. One such tool was the WHO's 2014 tool which has a primary focus on patients in the perioperative surgical journey. This specific tool was one of the newest evidence-based WHO instruments called "Patient's Communication Tool for Surgical Safety" (PCTSS) and composed of a structured, nine-item "Before Surgery" questionnaire. The communication tool consists of a nine-item questionnaire used to improve communication between the practitioner and the surgical patient. These nine questions ask specifics regarding patient's previous surgical procedures, fluid and food restrictions, pertinent health history, personal hygiene, medication history including supplements, whether a patient is pregnant or breastfeeding, medications to avoid preoperatively, the surgical location, their projected length of recovery and the pain expectations post-operatively.
Given that research and implementation tools developed by the WHO are well-known and respected in health care, I developed a project to use this tool throughout surgical units to improve communication during the surgical process. The goal was to decrease costs, surgical delays, cancellations, and postoperative complications. The educational questionnaire would help increase communication for preoperative patients about surgery, stress and anxiety levels, perceived postoperative goals, and aspects of a patient's perioperative experience. This questionnaire would also help patients to better relay their preoperative history so that their health care practitioners can fulfill the necessary requirements of their care before any surgical intervention is performed. The structure of the tool would also provide an open dialogue for a more highly effective communication between the doctors and patients, and any family members present.
The Challenge in a Low Resourced Setting
Improving patient safety is the primary reason to implement this project into the urban-city hospital's perioperative decision-making process. One of the long-term goals in utilizing this project was to position this hospital's pain division and anesthesiology department to be aligned with national leaders on the opioid crisis and patient satisfaction. The WHO questionnaire can save healthcare costs despite being a simple, low-cost tool. By reducing surgical delays and cancellations related to errors in obtaining a patient's past medical information, the goal of decreased surgical and anesthetic risks can be achieved by better communication. The project in turn could be a cost-saving method of reducing perioperative complications and medical mishaps associated with lost and misused healthcare allocations from communication errors while also enriching the communication between health care practitioners and their preoperative patient population.
Several barriers exist to establish a new process in a hospital environment. First and most challenging is to get approval from leadership or get &lsquobuy-in' that the process is legitimate and necessary. Second, once approval is obtained, training staff and individuals involved in implementation of the process is critical. However, given this particular hospital was under-resourced and staffing was a constant issue, many individuals were unwilling to take on another task to their already burdened daily duties. Third, assigning core leaders throughout the hospital who would implement the tool was another constant challenge. Communication with patients regarding surgery was key performance metric for leadership given hospital reimbursement was directly linked to patient satisfaction. Therefore, leadership understood that patient safety and satisfaction are paramount during patient care. Additionally, information collected during a preoperative assessment is generally used by the hospital's surgical and anesthesiology team to determine perioperative risks and usually does not get disseminated or coordinated with teams efficiently thereafter. Therefore, collection of data to improve processes long-term would be critical to sustain the program later which would be cumbersome given antiquated computer systems that existed at the time.
The importance of addressing this issue of opioid use, pain and patient satisfaction was critically important to leadership of the hospital given that reimbursement of payment of services was tied critically to the patient surveys. However, most team members felt more compelled to work with the project to address healthcare disparities in the hospital's most medically and socially vulnerable population in Philadelphia and the growing need to address the opioid epidemic particularly in this area was more of a secondary endpoint. Moreover, if outcome measures show improvement, a revamp of this Philadelphia hospital's preoperative education will be warranted and funding may be warranted. This eventually would bring long-term sustainability to the program and build the framework for a larger program in the future with staffing.
Improving Doctor-Patient Communication
When we used the tool in a pilot study population in Philadelphia to assess patient satisfaction, we found that providing this tool to engage the patient in the preoperative communication process may have an impact on overall outcomes especially in improving the awareness of complications which was statically significant (p=0.044). Many recent initiatives have stressed the importance of patient communication, both within healthcare teams and within the physician-patient relationship to improve the patient experience. This tool has the potential to engage patients further in ensuring their safety in the patient awareness of complications.
Conclusion and Implementation
There is a definite need for new strategies to counter adverse effects that hinder the quality of a person's overall surgical experience and outcome. Preoperative anxiety, especially during surgery, is associated with difficulties in establishing intravenous access, delayed relaxation of muscles, coughing and exacerbation of respiratory issues during induction of anesthesia, heart rate and blood pressure instability, and an increase in anesthetic requirements. Patient anxiety also correlates with elevated pain levels, increased nausea and vomiting risks in the postoperative period, a lengthened recovery period and an increased risk for advanced disease processes. These symptoms all increase healthcare spending through delayed patient recovery times. The implementation of the WHO's 2014 patient communication assessment through an efficient and well-coordinated project has the potential to enable patients to communicate more effectively with their healthcare providers, improving their awareness of the surgical process and hospital routine leading to improved postoperative outcomes and decrease the aforementioned complications. The financial impact of even small improvements in operating room efficiency is significant to a hospital with a busy OR schedule. A reduction in canceled cases increases volume and improves revenue in today's competitive healthcare environment. When surgical procedures are delayed, valuable OR time may be wasted, and staff time is under-utilized. This project is an excellent example of the benefits that prevention of complications affords and, "if at least five major complications are prevented within the first year of using the checklist, a hospital will realize a return on its investment within that same year". The opportunity for not only cost reduction, better surgical outcomes for patients with decreased stress and surgical fears, along with decreased numbers of surgical delays and cancellations should not be dismissed by administrators. Solving key public health problems often requires that healthcare practitioners use research-based knowledge, advocate for public policy changes and engage government agencies to implement change. In today's healthcare field, scientific researchers, clinicians, and policy analysts have become increasingly conscious of the crucial role that implementation science has in reducing the chasm between what has been shown to be effective in research and what is feasible in healthcare practices.
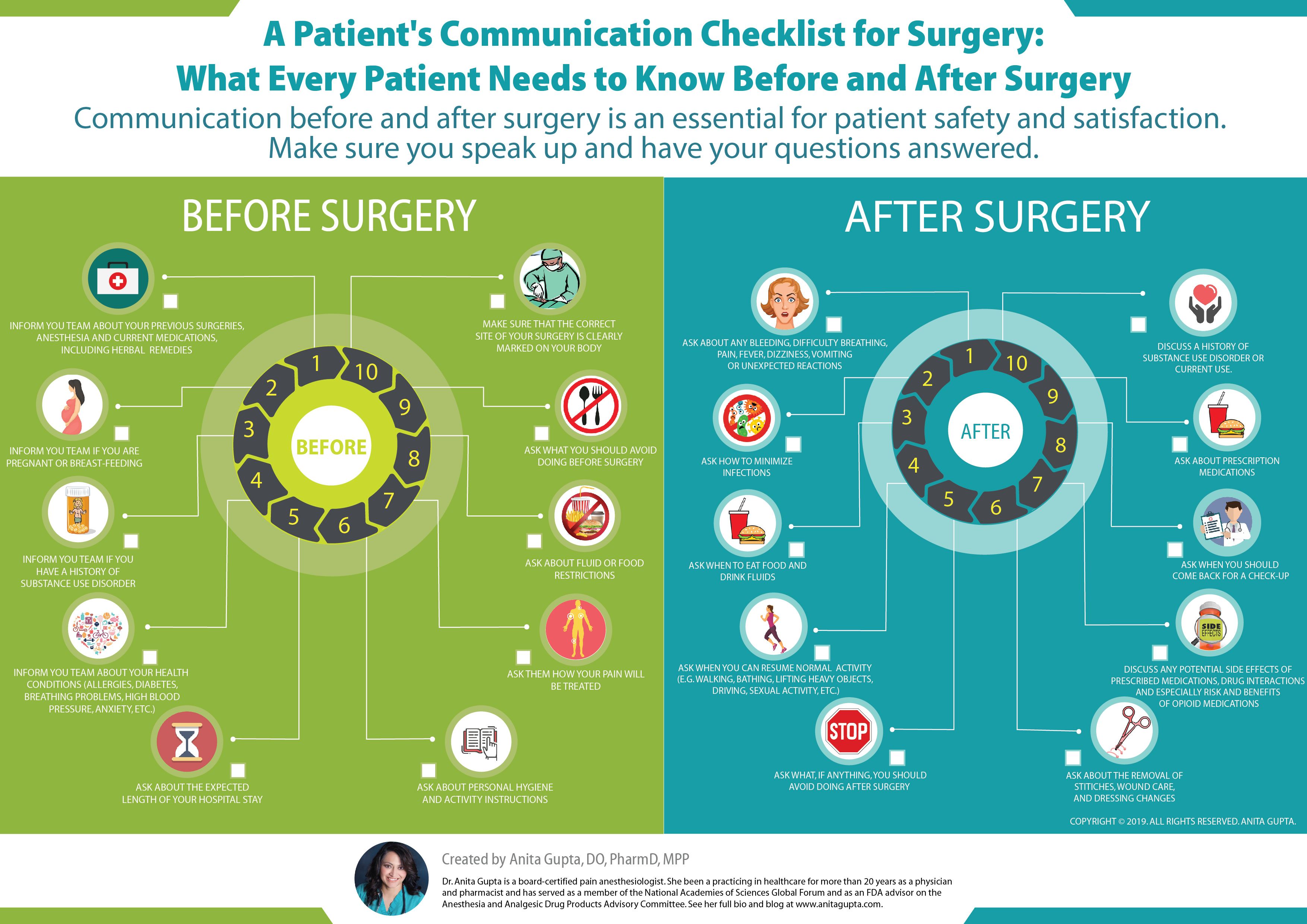
Here is a helpful graphic that shows the questions to ask before and after surgery.