Karen Roy had already survived an armed robbery that left her paralyzed at age 19 as well as the death of her husband, which left her a single mom to three teenagers at 47. Then, at age 53, she was diagnosed with urothelial bladder cancer (UBC).
“When you’ve gone through as much as I have — and I think I handled it all pretty well — I thought I was due for a break,” Roy said. “I had to rally myself for another fight.”
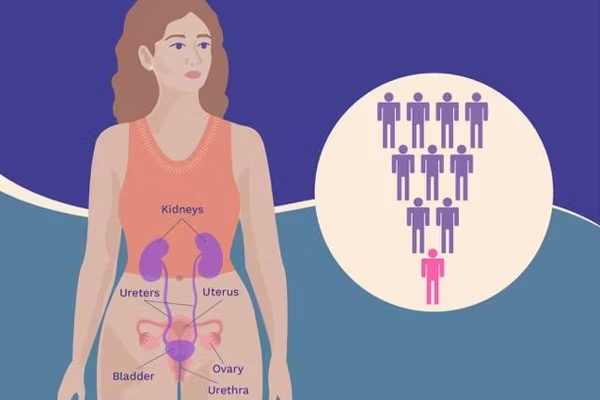
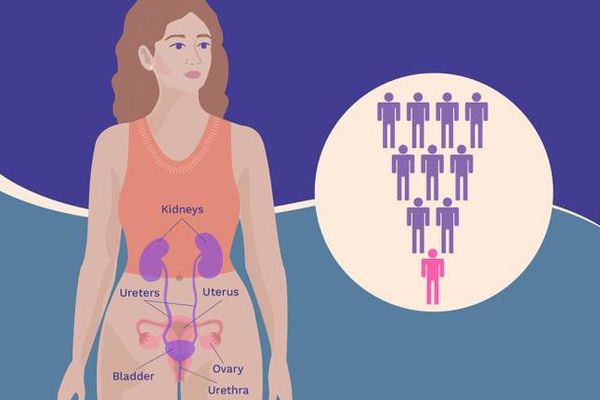
Like Roy, nearly 20,000 women in the United States will have their worlds turned upside down by bladder cancer in 2023. Understanding the ways UBC can affect your life may help you cope.
Treating bladder cancer takes a toll
UBC treatment can be intense and draining for patients, explained Sarah Psutka, M.D., a urologic oncologist and associate professor at the University of Washington School of Medicine. It can include everything from repeated minor surgeries to chemotherapy, immunotherapy and removal of the bladder (called a cystectomy).
“On top of that, there’s a [financial burden] associated with these frequent office visits and procedures,” Psutka said. In addition to covering the cost of treatment itself, many patients — especially those who must travel to receive care — also pay indirectly. “It’s time off work, it’s time for their loved ones who are traveling with them off work.”
Bladder cancer and mental health
The challenges of bladder cancer diagnosis and treatment can take a heavy toll on emotional well-being. “It’s a lot for patients to go through,” Psutka said. “And that has major implications for anxiety, depression, worry, treatment-associated burden and, ultimately, mental health.”
One of the many reasons people with bladder cancer may face mental health issues has to do with the possibility their cancer will come back.
The five-year bladder cancer survival rate is 77%, meaning about 8 in 10 people live for at least five years after their diagnosis. But bladder cancer is more likely to come back than any other type of cancer. Even after successful treatment, the rate of recurrence is between 50% and 80%. People with bladder cancer are also at increased risk of getting certain types of new cancers (called second cancers) later.
This means many bladder cancer survivors may feel like they’re walking around under a dark cloud of anxiety and fear about their cancer coming back.
In one survey of nearly 600 people living with bladder cancer, about 6 out of 10 said they feel anxious about their cancer returning, and about 4 out of 5 said they’ve searched “mental health and bladder cancer” online.
Because so many women are also caretakers, women with bladder cancer may also experience the special kind of anxiety that comes from worrying about who will look after their loved ones if something happens to them.
“I’m the sole parent of three young adults, and I help my mom who’s newly diagnosed with dementia,” Roy said. “I joke with my family about how I can’t die.”
How mental health can affect bladder cancer treatment
Although mental health is under-studied in relation to bladder cancer diagnosis and treatment, Psutka has seen the ways a patient’s mental well-being can affect how well they handle treatment.
“We do know that mental health has major implications for how patients tolerate therapy,” she said, adding that a patient's level of stamina and their ability to bounce back can impact their quality of life through treatment and beyond.
“I think that it’s probably an area that warrants a lot more research and attention from a research perspective,” Psutka said. “And it’s one of the reasons why we really have to pay close attention to our patients’ mental health as they're going through therapy and try to support that.”
Working through bladder cancer treatment
Keeping up with work while going through cancer treatment can be incredibly stressful — especially if you feel like you don’t have a choice.
With her whole family depending on her job for health insurance, Roy has been under pressure to keep working while having bladder cancer treatment. Even though she’s able to do much of her job at home, it isn’t easy to keep up.
“There’s this feeling of, ‘I’m the sole carrier of my insurance, so I better not get real sick,” Roy said. “I have a lot of fear and anxiety around that.”
Navigating relationships during bladder cancer treatment
For people with bladder cancer, navigating romantic relationships can be a challenge. Roy had just started seeing someone new when she was diagnosed. They went from spending their weekends at music festivals to spending them at the cancer treatment center.
“We were having fun,” Roy said. “Things got serious real quick.”
Insecurity about body changes during and after treatment can affect other kinds of relationships, too. People with bladder cancer may withdraw from their friends and turn down social invitations in favor of staying at home.
Advocating for yourself and connecting with others
Having learned at a young age the importance of advocating for your own healthcare, Roy — who hosts a podcast called “Life Possible with a Disability” about navigating life with a disability — understands the importance of finding a healthcare provider who will listen to you.
“Find a physician who is invested in your well-being,” she said. “Because it really is about your relationship with that individual physician and whether or not you feel comfortable with what they’re saying to you.”
Roy is also a big believer in leaning on others for support. “If people offer to help you, take them up on it,” she said. She also encourages women living with bladder cancer to reach out to organizations such as the Bladder Cancer Advocacy Network that can connect them with support groups and other resources.
“Speaking to other people who have gone through the same experience is really helpful,” Roy said.
Resources
Bladder Cancer Advocacy Network
This resource was created with support from Merck.
- It's Bladder Cancer Awareness Month: Time to Share My Story ›
- A Conversation With Dr. Sarah Psutka About Bladder Cancer ›
- Life After Diagnosis: Navigating the Things You Love with Urothelial Bladder Cancer ›
- Fast Facts: Everything You Need to Know About Urothelial Bladder Cancer ›
- What Women Need to Know About Urothelial Bladder Cancer ›
- Traveling During Treatment for Urothelial Bladder Cancer (UBC) - HealthyWomen ›
- Consejos para viajar mientras recibes tratamiento de cáncer de vejiga urotelial - HealthyWomen ›
- Sex After Bladder Cancer - HealthyWomen ›
- Doctor’s Dismissed My Bladder Cancer Symptoms as UTIs - HealthyWomen ›
- Ask the Expert: Urothelial Bladder Cancer - HealthyWomen ›
- Vivir con cáncer de vejiga - HealthyWomen ›
- Mental Health and Urothelial Bladder Cancer - HealthyWomen ›
- Going Back to Work with Bladder Cancer - HealthyWomen ›
- Regreso al trabajo con cáncer de vejiga - HealthyWomen ›
- Los sobrevivientes de cáncer de vejiga y los segundos cánceres primarios - HealthyWomen ›
- Bladder Cancer Survivors and Second Cancers - HealthyWomen ›
- Bladder Cancer and Black Women - HealthyWomen ›
- El cáncer de vejiga y las mujeres de raza negra - HealthyWomen ›
- Urothelial Bladder Cancer Quiz - HealthyWomen ›
- Cuestionario del cáncer de vejiga urotelial ›
- Q&A About Urothelial Bladder Cancer Treatment - HealthyWomen ›
- Preguntas y respuestas relacionadas con el tratamiento contra el cáncer de vejiga urotelial - HealthyWomen ›
- Diagnosing Urothelial Bladder Cancer (UBC) - HealthyWomen ›
- The Start and Spread of Urothelial Bladder Cancer - HealthyWomen ›